Whenever you experience an injury or have a niggling pain in your lower back, you probably decide to completely rest up so that whatever ails you can heal and recover. But the pain doesn’t go away, so you introduce some light isolation movements to help with the recovery. But the pain still doesn’t go away, so you rest some more and pretty soon it’s been months or even years since you’ve done anything that resembles real exercise.
My guest today argues that if you want the pain to go away, you’ve got to get off the Barcalounger and under a barbell.
His name is Dr. Darin Deaton. He’s a physical therapist, CrossFit coach, and Starting Strength coach. Today on the show, Darin and I discuss the common myths people have about the safety of barbell training and why family practitioners and physical therapists contribute to the existence of those myths. Darin then explains why strength training is the best tool for rehabbing an injury and why the reason you have a bad back in the first place is because your back isn’t sufficiently strong. Darin and I then discuss his overall philosophy and approach for rehabbing patients utilizing barbell lifts as well as other physical therapy modalities. We then get into specific injuries that barbell lifters and runners experience and how to rehab them. We end our conversation discussing the effectiveness of practices like dry-needling and electrical stimulation in recovering from persistent pain and injuries.
Show Highlights
- Darin’s background and he came to be a physical therapist and Starting Strength coach
- Why PTs and barbell training don’t always go together, and how Darin bridged that divide
- Myths about barbell training that persist in the health care world
- Do back injuries totally prevent people from barbell training?
- How barbell training helped Darin recover from his back surgeries
- Why being overly cautious just reinforces your weaknesses
- The most common injuries that Darin sees in his strength coaching
- What the American Academy of Pediatrics (AAP) says about kids and strength training
- Does strength training stunt development in children and teenagers?
- What your training should look like after an injury
- The unconventional Starr rehab model
- How to treat common running injuries
- What is dry needling? How about cupping? What use do those have in rehab?
- Is there a way to know when an injury is healed and you can resume full training?
Resources/People/Articles Mentioned in Podcast
- Podcast: My Workout Routine and the Benefits of a Strength Coach
- Starting Strength by Mark Rippetoe
- Practical Programming by Mark Rippetoe
- My podcast with Jordan Feigenbaum
- My podcasts and videos with Mark Rippetoe
- AoM articles, videos, and podcasts about barbell training
- Podcast: Undoing the Damage of Sitting
- AAP: Strength Training by Children and Adolescents
- How to Instill a Love of Fitness in Your Kids
- The Starr Rehab Method
- Dealing With Bicep Tendonitis
- My podcast with Jason Fitzgerald on runners and strength
Listen to the Podcast! (And don’t forget to leave us a review!)
Listen to the episode on a separate page.
Subscribe to the podcast in the media player of your choice.
Podcast Sponsors
Athletic Greens. The most complete, whole foods supplement available, plus it tastes fantastic. Head over to AthleticGreens.com/manliness and claim your 20 FREE travel packs today.
Indochino offers custom, made-to-measure suits at an affordable price. They’re offering any premium suit for just $359. That’s up to 50% off. To claim your discount go to Indochino.com and enter discount code “MANLINESS” at checkout. Plus, shipping is free.
Casper Mattress. Get a better night’s sleep without the usual hassle of mattress shopping. Get $50 toward any mattress purchase by visiting www.casper.com/MANLINESS and using offer code MANLINESS.
Click here to see a full list of our podcast sponsors.
Recorded with ClearCast.io.
Read the Transcript
Brett McKay: Welcome to another addition to the Art of Manliness podcast. Whenever you experience an injury or have a niggling pain in your lower back, you probably decide to completely rest up so that whatever ails you can heal and recover. But then the pain doesn’t go away, so you introduce some light isolation movements to help with recover. But the pain still doesn’t go away, so you rest some more, and, pretty soon, it’s been months or even years since you’ve done anything that resembles real exercise. My guest today argues that if you want the pain to go away, you’ve got to get off the Barcalounger and under a barbell.
His name is Dr. Darin Deaton. He’s a physical therapist, CrossFit coach and a Starting Strength coach. Today on the show, Darin and I discuss the common myth people have about the safety of barbell training and why family practitioners and physical therapist contribute to the existence of those myths. Darin then explains why strength training is the best tool for rehabbing an industry and why the reason you have a bad back in the first place is because your back isn’t sufficiently strong. Darin and I then discuss his overall philosophy and approach for rehabbing patients utilizing barbell lifts, as well as other physical therapy modalities. We then give the specific injuries that barbell lifters and runners experience and how to rehab them. We enter a conversation discussing the effectiveness of practices like dry needling and electrical stimulation in recovering from persistent pains of injuries. After the show’s over, check out the show notes at AoM.is/Deaton.
Darin Deaton, welcome to the show.
Darin Deaton: Thanks. Thanks for having me.
Brett McKay: You and I, we met a few years ago at a Starting Strength seminar because you’re a Starting Strength coach who was auditing the seminar. It’s one of the requirements. We’ve interacted before then, but you’ve got an interesting background. Besides being a Starting Strength coach, tell us a bit more about yourself and what you do.
Darin Deaton: Sure. So I’ve been a doctor of physical therapy for 28 years. I’m the founding partner of an orthopedic and neuro physical therapy practice group, Dallas/Fort Worth, North Texas area. I’m also a Starting Strength coach. I think I’ve been a Starting Strength coach since 2012 or ’13, and I’m Starting Strength’s staff, on the seminar staff, teach at some of the seminars. I’m also a USAW Sports Performance coach and also a CrossFit, what they call level three trainer, so I’ve gone through three different levels of their coaching training. I’ve had a varied background in fitness. My wife and I actually met over 30 years ago when I was … actually, 31 and a half years ago, when I was 19 years old in a health club. I was a personal trainer of sorts, and she worked there also, and that’s where we met, there and at junior college when I was taking some summer classes.
I’ve been in the fitness industry for over 30-plus years. I’ve been in physical therapy for close to that too. The background that I have in relationship to the lifting community is more specifically with Starting Strength. I’m also a Starting Strength online coach on the Barbell Logic Online Coaching product that Matt Reynolds started a little over a year ago, which is a great product for lifters who don’t have access to a personal coach, one-on-one, and a physical presence. It’s great to have good eyes on coaching. That’s about my background.
I think that I’m a little different in the sense that … And so are my clinics. I have two partners in my practices. We have four different locations here in the area. In our practice, we have a barbell rack or a squat rack, I guess you would say, a power rack, barbells, upper plates, steel plates. We use a lot of traditional barbell training in our clinics for strength training because we feel like it’s probably the most effective tool that we have at our hands. That’s pretty much it.
Brett McKay: Barbell training, your primary practice, which is weird because you’re a physical therapist. I’ve been to the seminar. I’ve … at the seminar, rip … pretty much went after physical therapist like they don’t know anything. So how did you, a physical therapist, get into barbell training, particularly Starting Strength?
Darin Deaton: Basically, I went to the Starting Strength seminar, I think, in 2012. That’s when I got my certification. I got my certification at the same time. I attended the first seminar, sat for the platform test, passed the platform test and the exam, and then became a Starting Strength coach. But there was a period of time there for probably at least three to four years where I did very little within the community of Starting Strength, just because of my practice life was busy. I had CrossFit gyms. I’m a big reader when it comes to strength, and so I kept reading. I’ve read Starting Strength, The Barbell Method, and then also Practical Programming, and there are several other texts. They just continued to intrigue me, so I continued to follow it.
Later, I ended up getting involved again back with the Starting Strength community. I’m not on staff as a staffer, do staff some of the seminars. But as you know, when you go to the seminar, PTs are not held in a very high light, and, in a lot of ways, they earn that because of the way that we have talked about strength training and barbell training within the medical community. It’s hard to survive as a PT in the Starting Strength community. You have to have pretty thick skin, but I think that it makes sense to me. Barbell training’s very methodical. It’s very predictable. Also, from a science standpoint, when you think about physics and moment arms and loads and force production, it just makes sense to a didactically thinking mind, someone who is very analytical. It makes sense, and so I couldn’t get rid of that.
The more that I learned, the more that I got around other Starting Strength coaches and Mark Rippetoe, the more I realized that this is really the method that I want to promote as the primary strength training model, both in my clinics and also in my gyms.
Brett McKay: So let’s talk about some of the myths that exist in the medical field, but particularly the physical therapy profession because we’ve had Jordan Feigenbaum on the show, who’s a medical doctor, also a Starting Strength coach. We talked about some of the myths that even just family practitioners have about barbell training in particular. What are the big ones you see in the PT world about weight training or barbell training in particular?
Darin Deaton: First, I think the average customer or client of the medical community needs to understand that, when it comes to strength training, when it comes to the development of strength, PTs definitely get more academic training than medical physicians, both DOs and MDs do. But physicians get very little education when it comes to strength training, endurance training, just anything outside of medicine. The idea that a physician would be the expert in that field or even the physical therapist is probably not accurate. But a lot of the misconceptions that are out there is, first of all, when it comes to the barbells, that the movements are dangerous, that you should isolate movements, that you should do individual exercises that are smaller movements. There are some cases where we have to be careful with patients, when we’re talking about the care side, postoperative care, injuries where there’s structural issues. Then there are certain times where we have to be careful about how we intervene with those exercise activities.
But there is a significant difference, as you know, between exercise and training. I think it’s important that people recognize that the barbell is probably, in my mind, at least … and I think in a lot of the minds of a lot of strength coaches and several PTs I know and physicians, like Jordan and Austin Boraki, who’s also a physician, Dr. Jonathon Sullivan. That would be that a barbell can be a great tool. It’s very safe. A lot of people think it’s not safe, but it’s extremely safe. It promotes compound movement versus isolated movement, and we know that compound movement is safer to the joint because it stabilizes the joint. It stabilizes the surrounding tissue, if that makes sense.
Brett McKay: Got you. I mean, whenever I’ve preached, hey, to people, you need to get started with barbell training, I’ve had a lot of guys, particularly older guys in their 40s or 50s, they say they’ve got a bad back. Is that something that can prevent people from barbell training if they’ve got a bulging disc or something like that? What goes on there? What’s your prognosis as a physical therapist?
Darin Deaton: No. I think that the last thing that someone needs to do is stop strength training, when it comes to a back injury. A strong back is a healthier back, and we know that through the literature now and through research that a back that’s weak hurts more. Backs that have larger musculature, better stability and support. It supports the tissue that’s been damaged. It supports the disc, the ligament and structures and the spine itself. I don’t tell too many people this, but most of the people that hang around with me in my circles know this. But two years ago, I had four low back surgeries in the same calendar year. I had three laminectomy discectomies, at the same level, and then I eventually had a lumbar fusion had L4-L5. So as a PT, when you think about that, the myriads of patients that I’ve treated all these years, that was pretty discouraging. But I had a condition called spondylolisthesis. I had an unstable segment. The only way to finally take care of that was through surgery.
I’ll just tell you that getting back under the barbell over the last two years has been the best thing that I could have ever done for my back. The other day I squatted for three sets of five, my old PR for a single rep, prior to back surgery. I’m deadlifting for a set of five what I use to PR. When I talk to clients, specifically patients, but also members that were within our gyms or when I had one-on-one clients through strength training sessions, I’d tell them there’s a lot of misconception out there about lifting weights and bad backs. If your physician or within the community that you hang around with, if they tell you, you don’t need to be lifting heavy weights anymore … The one thing we hear all the time is … You’ve probably heard this, Brett. Don’t lift more than 10 pounds, right? I mean, don’t lift than 10. You never lift anything more than ten pounds. Don’t ever bend over. You should squat with your legs only.
You and I know that that’s not the proper way to use the hip and the back. It’s a lever, so it should be used as a lever. That back needs to stay straight, but the hip is the driving force for that, the hip, the glutes, the hamstrings. What we try to do with our patients now in our clinics and what I try to do with my strength training clients is help them understand anyone can lift a barbell and get stronger in the hips and low back. A lot of back pain is what we call nonspecific back pain, and the best way to treat that is with strength training.
Brett McKay: I think that’s a great point because I’ve read that in other places. There’s research on Home Depot employees who wear those back braces. They tend to have more back injuries than people who don’t wear the braces because they’re basically relying on that belt to act as an exoskeleton for them, so they get a weak back. Then whenever they’re at home with the thing off and they pick up a load of laundry, they pull their back, and then they’re out for a while.
Darin Deaton: I think there’s this mindset or this thought line that’s created that can be pretty pervasive, and that is you shouldn’t use your back this way, or you shouldn’t use your back this way. I think they develop a mindset that you have to be careful with your back. Well, sure, you have to be careful with a lot of things, but being careful and assessing risk is different than being just cautious about things. Some people are just so overly cautious, they develop weakness. I’ll give you a good example. I had a patient this morning that I treated that’s a postop shoulder patient. It’s very similar to the same situation with the back patient, and that is his physician told him I don’t ever want you to lift overhead again with your shoulder.
My question to that doctor might be and to that patient might be, well, did the physician feel like that he got a good repair in your shoulder, a good, what we call, purchase of the hardware or the tendon or whatever he repaired in the shoulder? Well, the patient said, “Yes.” He said, “My shoulder was the perfect shoulder to perform this procedure on.” If the shoulder joint is designed to raise up over your head, why wouldn’t you go back to strengthening it in that method and use it? It just functionally makes sense. Well, the same with the back. The only difference is, with the back, a lot of people don’t know how to lift. They don’t recognize how to use the hip, and they definitely do very little strengthening on a day-to-day basis, when it comes to the low back.
Brett McKay: Let’s say someone who’s never lifted before, they’ve got an issue like that, either an issue with their back or a shoulder. I know shoulders are very common with folks. As a practitioner and as a coach, how do you go about introducing them to barbell training?
Darin Deaton: It matters where I see them. If I see them in a clinical environment, the approach is … It’s similar, but I’m in my medical world there, if that makes sense. Let’s say a physician has ordered PT for the patient, prescribed PT, and I’m seeing them because they had a lumbar sprain and strain, or they have a bulging disc or what they would call a quote, unquote “bad back.” I might treat them a little bit different, but we still go into education. We talk about using the hips as a lever. We talk about using the back in a straight angle, that the back stays in a nice, locked, straight position when we lift. Then we go through, and we start teaching them how to deadlift, how to back squat. I teach them the overhead press too because that builds the midline stability, the core strength.
Then we gradually also add other assistive exercises in also, but a lot of people, when they think of spine strength, they think of the abs. I’m going to do sit-ups to get my abs strong, right? The problem with that is that’s not how the spine and the abdominal wall actually functions on a day-to-day basis in the human body. It’s mostly an isometric muscle group. It’s a group of muscles that stabilize the spine through isometric contraction throughout the day. Then when you volitionally want to use the spine to lift something heavier, then you Valsalva. You tighten up. You keep that back nice and straight, and you hinge at the hip. Those are the kind of things that we teach. The number-one thing is I educate them on the front end that this is the proper way to use your hips and your back. You can be lifting. You can get strong over time, and you can stronger probably than you ever thought you could be. But the biggest limiting factor is going to be their mind; we’ve got to change their mindset.
So we gradually work them through their rehab program, if they’re a patient. Then I put them into a barbell program, give them some basic level programming. They can either do that on their own in a local gym, or they can then come and see me as a strength coach, and we’ll work with them one-on-one and then put them on a program also.
Brett McKay: Got you. So the bottom line is, if you have an issue and you’ve been leery of getting into strength training but you’ve been wanting to, don’t be afraid. Go seek professional advice. But what do you do? You go to a PT who’s not a Starting Strength coach, and they’re going to give you the typical advice of here’s a soup can, and do a shoulder … What do you do if that’s what they prescribe?
Darin Deaton: In every community, there’s a differing level of expertise in every single community. Years ago … I’ve been in the fitness industry … My wife and I met when I was 19 years old in a health club, where I was a quote, unquote, “personal trainer.” I’m not real sure what I knew back then, but I was personal trainer. But in every industry, we have varying levels of expertise, and so I wouldn’t say necessarily because a physical therapist is a licensed PT that they actually possess the knowledge or the experience base to do the type of strength training that I think is effective or that you might think is effective now, based on the fact that you do Starting Strength. It’s difficult sometimes. You’re not real sure what you’re going to get yourself into.
But I can say this. If you’re a patient and you’ve been treated for low back pain and you’re not getting the results that you want from your physical therapist or your doctor or whoever you’re seeing, your chiropractor, whatever medical professional or alternative medicine person you’ve sought, you can go to StartingStrengthOnlineCoaching.com, and you can seek out a Starting Strength coach. I can say this, that every single coach that’s on that staff has an expertise level on how to do barbell training and could probably help you work through your back pain and getting back to a healthy, strong back, where you can live a successful lifestyle. That’s one thing I know for sure.
In a local sense, if you’re dealing with a physical therapist that you feel like you’re not making the headway that you want to make, then reach out to Barbell Logic Online Coaching. You could also reach out to me, and I could hopefully find you someone in your area that’s a little bit more strength-minded as a therapist. Most physical therapists, they mean well, and I think there’s a lot of great physical therapists out there that are very strength-minded today. We do see a trend in the world of physical therapy to move toward a more active, strength training mindset, a more preventative mindset. But we still have a lot of physical therapists in our community too that they’re just not effective in their ability to create true muscle hypertrophy strength and adaptive change in the patient.
Brett McKay: So we had Jordan Feigenbaum on the show, Dr. Jordan Feigenbaum on the show. He highlighted the research that basically shows that weight training is probably one of the safest activities you can take part in. You’re more likely to get injured playing soccer than you are lifting weights. With that said, it is possible, in the process of your training, to get banged up, experience injuries, some hurts. In your experience, as a coach and as a physical therapist practitioner, what are the most common … I don’t know if you want to call them injuries or just dings to the body that you see whenever someone’s barbell training?
Darin Deaton: I think the thing we see the most would probably be low back sprain and strains, a lot of times. If you’re doing any type of training, it’s not if an injury’s going to occur; it’s really when. When in your training career, your training life, are you going to get injured? I mean, you can get injured bending over and picking up a pencil, and probably it has happened through cumulative trauma over time, improper lifting, lack of strength in that segment, lack of activity in your lifestyle, maybe a sedentary lifestyle. There are a lot of things in life that cause injuries, but the most common injuries that we see would be low back sprains and strains, shoulder sprains and strains that would probably eventually show themselves as rotator cuff injuries, most likely. Growing strains, like an adductor strain through squatting, hamstring strains and sprains, and then also sometimes we see some bicep tendonitis, elbow tendonitis from barbell training, just like we do any other type of training. But like you said, the injury rate in barbell training is extremely low.
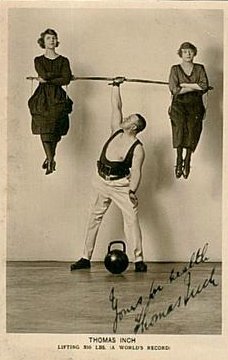
This is an interesting just little tidbit of information. Years back, it’s been two or three years back, I was doing some studying on Olympic weightlifting. You know what Olympic weightlifting would … That would be the clean and jerk and the snatch. That’s a dynamic effort that’s speed-based, that’s power-based, strength-based, but there’s a lot of movement in a very broad range of motion. It’s even less predictable than barbell weight training, where you’re doing, let’s say, the press, the bench press, the back squat and the deadlift. I was doing a study probably two or three years back because I was talking to some parents about using Olympic weightlifting for dynamic effort explosiveness for younger athletes.
At the time, I believe it was the American College of Pediatric Medicine had come out with a position statement, working with Dr. Kyle Pierce, who works with USAW, to support … They eventually said that, if a child, if an adolescent was going to strength train or do a strength training program, then a safe way to do it would be something like Olympic weightlifting because, number one, it’s coached. Number two, it’s predictable, and, number three, it’s something that can be linear-based. You can gradually increase the loads over time as technique improves and as strength improves and expertise. I think about that in this format. If Olympic weightlifting is that safe for that young population, how much more safe would just classical barbell training be, where there is not as much speed, there’s not as much dynamic effort? It’s more a controllable motion.
That’s the one thing I love about barbell training, is I know that when my client walks into the gym or into the clinic that next day, I know exactly what they’re going to do, how they’re going to do it. I know the set, rep scheme. There’s no unknowns. To me, to be able to do that and to track that over time, day in, day out, there’s this gradual, progressional, linear model that’s developed that creates strength, and the other thing is the connective tissue. The connective tissue gets gradually stronger over time, so the likelihood of an injury is much less apparent than if I just went in and did some random exercise workout, if that makes sense.
Brett McKay: Right. You just go into the gym. You go to all the different machines in a random whatever.
Darin Deaton: Yeah. I think people have a misconception about barbell training because, let’s face it, you go into any larger Globo Gym, you go into any facility, and you see people doing things that … Well, you know now, based on being trained in a classical barbell program and having a great coach. You know now that there’s a certain way to lift a barbell. There’s a skill, right? It’s not random. It’s very specific, and it’s very methodical. Well, there’s a lot of stuff that goes on in gyms that you just have to roll your eyes at. It’s not good training. It’s not training at all; it’s exercise. Like Rip says, exercise is getting hot, sweaty and tired, but training is outcome-driven. It’s specific, and we’re doing something to create a change in the human body, whatever that change is, whatever that physiological change it.
That’s the beautiful thing of barbell training, and that’s why I think it can be so effective in a rehab model too, is because it is predictive, because the patient or the client gradually increases over time, just like they would in any other rehabilitation program. We just happen to be using the barbell more often. Our clinics, all four of our clinics that we presently have, have barbells in them. We have standard weights. I guess, you would say plate weights. We have everything from fractional plates to 45-pound plates, and then we also have squat racks, power racks in each one of our clinics. Our therapists use that … Some therapists use it more than others, but you’ll see that most of my patients use the barbell rack. Almost every single patient will have some application with it.
Brett McKay: There’s a lot to unpack there with some of the stuff you said. I want to go back to the kids and weightlifting because that’s a question we often get. People want to get their kids with weightlifting, but they’ve probably heard the rumor, the old wives’ tale … Is that when you say that, they’re called nowadays? That it stunts their growth because it somehow damages growth plates. Is there anything true to that, or is that a bunch of bunk?
Darin Deaton: No, I mean, that’s a bunch of bunk. I think there is an age, as they’re going through their stages of development, their skeletal development, where we have to be more careful than other ages. But with younger clients, let’s say clients that are 12, 13, 14 … Let’s just say 13, 14 year olds. Not all 13 year olds have the same skeletal development as all 13 year olds. There’s a difference. They may be a little bit farther into puberty. They may have more skeletal development. They may be carrying more muscle mass. You can have a 13 year old that’s very underdeveloped, and you can have a 13 year old that’s 6’1” and 200 pounds and very developed, physiologically or physically in regards to skeletal structure.
The key thing we do with younger clients is, first of all, we teach them form. We teach them how to move the barbell, and that’s built off of repetition and coaching, so in cuing and teaching them. We teach them first. We cue them, and we coach them through all those movements to make sure that they’re sound and safe. Let them have fun while they’re in the gym. Then a little bit later in life, then we gradually start adding load and put them into a novice linear progression. But I think the safest method to develop strength in some of these younger athletes, which is not being done very well in high schools today, would be to put these young athletes, these 13, 14-year-old athletes into a sound, novice linear progression and then just gradually increase that strength over time. If these strength programs would do that, by the time these kids got into high school, some of the numbers would be unbelievable in regards to their strength capacity. I think that would roll into their ability to perform their sport.
When it comes to what people think kids need for their sport, we don’t need to train them specific to their sport when it comes to strength. We just need to get them strong. We get them strong, then the sport-specific coach can deal with all the sport-specific issues that come with that sport. But our goal, as strength coaches, is to get them a good foundation of strength, and then they can use it for whatever they want to use it with.
Brett McKay: Let’s backtrack. You said some of those common injuries that you might experience while barbell training is sprained backs, lower back pain, bicep tendonitis, something I’ve dealt with, shoulder stuff. What happens? Let’s say you get the back thing. You’re doing a deadlift, and while you’re pulling, you tweak your back. Do you freak out? What are the immediate steps you should do to start rehabbing that? Should you stop training altogether? What’s your approach?
Darin Deaton: The last thing I want to do is stop a client, whether they’re a patient or just a strength client, from training or to stop moving. The other Starting Strength coaches and just some of the people that know me in professional circles, I always use the term motion is lotion. You’ve got to stay moving. It’s good for the human body. We want increased blood flow. There’s a misconception that you injure your back, well, you should stop doing anything for sometimes a prolonged period of time, and that’s farthest from the truth. Now we know that you should probably get back under load. How you get under load and when you get under load and how much you load is determined based on what type of injury it is. Is it an injury, or is it just hurt? There’s a lot of little tweaks that occur along the way. You get a little sprain and strain here, or you get a little soreness here. You get a little hurt, quote, unquote. Well, that’s different than being truly injured.
What you want to do first is you want to seek the help of someone who has a diagnostic background. I prefer that you seek a sports medicine physician. If it’s a minor injury or a minor sprain and strain, then it’s something probably that you can take care of yourself. You want to ice the injury directly after the injury. You want to stay moving though, and you eventually want to get back underneath that bar, if you’re barbell training as your strength method. The key there is we do need to get, in some of these cases, some form of diagnosis done. I just say that as a … I put my white coat on there. That’s not my strength coach coat. If I put my white coat on, then an accurate diagnosis upfront is important.
Let’s say you went to your family doctor or a physical therapist, based on what state you live in, and you got the diagnosis of a lumbar sprain and strain. They’re going to tell you stop lifting for a while. Don’t barbell train. That’s not what I would have you do. What I would have you do is we would gradually go back into lifting. We might even use a rehab method called STAR Rehab Model. The STAR Rehab Model is using higher rep scheme with lower loads and body weight loads to gradually increase the blood flow to that area, just infuse that area with blood flow so that we can increase the nutrients, increase the healing agents to that area. Then we just linear progression, gradually increase the load over time. Get you right back into training very quickly. Instead of just hoping the body heals, in a roundabout way, we force the body to heal.
Brett McKay: That makes sense. Let’s talk about tendonitis because I see this one. This probably pops up for older guys, in particular, because when you’re young, you’re supple, right? When you get older, you get a little stiffer, and things aren’t as pliable. First of all, why does bicep tendonitis happen, and what do you do to train around it?
Darin Deaton: Any tendonitis, it matters what we’re talking about here. There’s three stages of tendon injury. We’ve got tendonitis, tendinosis, and tendinopathy. A tendonitis is basically just inflammation of the tendon. There’s been an inflammatory process. There might be very little damage actually done to the tendon, but the tendon’s inflamed through an overstretch, an overstrain or overuse. It could be overuse swinging a hammer, or it could be from lifting.
A tendinosis is, once we’ve had several tendonitises or we’ve had several smaller injuries, then there’s an actual structural change to the change belly itself. The tendon cells that are in there have some scar cells in there now, and it’s just not as healthy of collagen because collagen tissue’s what your body’s made out of, and the tendon cells are not as resilient. That’s what happens with some older athletes or older lifters. They get tendonitis from overuse or this sprain or this strain, and then it ends up being a tendinosis. Once it gets warmed up, it feels really good, but before you get it warmed up or maybe on a cold day or something like that, it’s achy and uncomfortable, but once you start using it, it feels pretty good. Then the last thing would be a tendinopathy, and that’s where the actual tendon tears, and there’s a structural weakness in the tendon. Eventually the tendon could rupture like a distal bicep rupture or a patellar tendon rupture, Achilles rupture. That would everybody the worst thing that could happen because it completely detaches.
The way that I treat tendonitises, tendinosises and tendinopathies is a little different based on the severity of the injury. The rehab model’s going to be different based on the severity. Let’s say we’re dealing with just a classical tendonitis, the first thing we want to do is we want to make sure that we’re using that tendon. We may have to reduce the loads for a period of time because of the structural inflammation that’s there, so we’re going to use things like ice, do transverse friction massage. Sometimes it’s appropriate, sometimes, to use a corticosteroid injection in that area or to use things like iontophoresis, where we use a topical steroid. They also might be taking NSAIDs, non-steroidal anti-inflammatory drugs, to reduce the inflammatory process in the tendon. The last thing we’re going to do is not use the tendon.
I’ll tell you this is a really interesting case. I was treating a guy this morning, or one of my colleagues was treating him, and we were just talking about him together and working together on him. He’s had a medial epicondylitis, which is a tendon inflammation of the medial elbow. Thing’s also called golfer’s elbow. He basically has had this for about two or three years. He’s had multiple injections to the area. This is obviously a tendinosis. He’s got some adaptive tissue changes in that area. What the therapist and I have been working on is to start doing some eccentric chin-ups with him, start doing some eccentric curls with him, and start to really load that tendon with eccentric activity, higher reps, body weight loads and lower loads, with just really flushing that tendon belly with blood, expanding that tendon with blood products and lubrication so that it can heal itself as best possible. We also recommended something like an elbow sleeve with him, to keep it warm so that, when he’s at work and he’s not using it, we’re keeping that body temperature in that area a little warmer. What he’s noticed over time is that it’s actually getting better; it’s improving.
The number-one thing we want to do is we want to keep these patients moving, or these lifters moving. We might have to alter load and weight, reduce it, but we’re probably going to use a higher-rep scheme with more sets. We’re going to use eccentric training too, along with that, and then all the other things that we talked about, NSAIDs and ice and friction and some of the sideline therapies we can use. We could use e-stim on it, those types of things.
Brett McKay: Darin, do you treat a lot of runners, by chance?
Darin Deaton: I mean, we treat a fair amount of runners in our practice. We see quite a few.
Brett McKay: What do you think are the most common injuries you see with those guys?
Darin Deaton: Oh, probably Achilles tendonitis is real common; planar fasciitis is real common. Some of them will get some nonspecific knee pain, will get some achy knees from having a little arthritis in the knees, hip flexor sprains and strains. Sometimes they’ll get a little patellofemoral pain from running with improper form or if they’re running hills or trails, those types of things.
Brett McKay: Is your general philosophy towards those guys too is keep them moving? You’re not going to stop running. You might just change the way you train.
Darin Deaton: Yeah. I think with a runner, it’s a similar philosophy. The number-one thing I’m going to do is I’m going to look at their strength base too. If they’re under strength … And runners are classically weak as athletes. If they lack strength, which they probably do, I’m going to put them in a classical barbell training program. We’re going to get them under the bar, and we’re going to get them stronger because, a lot of times, runners have injuries because of form breakdown and form creep throughout their run. They get tired. They lack the stamina that they need to run with proper form. We may need to address their form. We need to address the way they run, their shoe wear.
With a runner, what I might look at is volume too. A lot of runners can be classically over users. They can over train. We’re going to look at how much they’re running. One of the things that I’ve done over the years, and some of this came from my background with CrossFit, and that is learning how to use high-intensity interval training or interval running to improve aerobic and endurance capacity without running the high volume that a lot of runners or that a lot of triathletes or endurance athletes normally use. We’ll work on … Let’s say in the past they’ve used three long runs a week or five long runs a week. We might then come in and change their training model. Let’s do some high-intensity interval training on this day. Let’s do some sprints, or let’s do something like the Assault bike and maybe do interval sprints on the Assault bike and give your … We’re still working the hips and legs. We’re still working their cardiovascular system, but what we’re also doing is give their body a little rest from the pounding, if that makes sense.
The thing we look at with runners would be we check out their training program, the volume that they’re running. We look at their form. Then what we’re going to do is probably put them into a strength program because it’s predictable, get them strong, make sure that we’re strengthening that connective tissue. Then we can do all the things that we talked about earlier with tendonitises and other injuries, using modality care and physical therapy to reduce the inflammatory process along the way and get them back to running.
Brett McKay: This is a personal question related to running because I experience this. I think two years ago, yeah, about two years ago … no, a year and a half ago, I did some wind sprints for the first time in a long time.
Darin Deaton: Boy, that’s painful.
Brett McKay: It was pain- … So, yeah, I think what happened was, after the next day, on my left hamstring, up near my butt, it was just this pain. It just hurt all the time, and I think it was some sort of tendonitis, like the hamstring … Is there a tendon there-
Darin Deaton: Yeah.
Brett McKay: … by chance?
Darin Deaton: Yeah.
Brett McKay: Just until fairly recently the pain went away, but it took a long time. What do you do, if you’re a runner and you get tendonitis there? Because I think it might be a hard place to treat.
Darin Deaton: Yeah. I mean, the hamstring comes up to what’s called a conjoined tendon. It’s where the hamstrings all convert back up in there, and they attach on the ischial tuberosity. It’s the sit bone; it’s what you sit on.
Brett McKay: It’d really flare up when I was on a long road trip. I’d get out of the car, and it’d just hurt so bad.
Darin Deaton: You go to stand, and you’re like, oh, my gosh, that’s killing me. You start having to use that hamstring again. I mean, something like sprinting is perfect to injure that, if you haven’t been sprinting. Here’s the thing you’ve got to watch, sometimes, is that, when you’re doing something like that, like high-intensity interval training, sprinting, there’s a ton of sport hormones going on in your body. Your body temperature … I mean, you’ve got everything warmed up. Everything feels great. Really, a lot of those hormones that are rushing through your body at the time, they’re designed to reduce pain. They’re designed to reduce the nocieception, the pain response in your body. Then you get a little overuse, and there’s an inflammatory process. You may have not torn the tendon, but you may have irritated its origin or the insertion down near the knee, when you’re talking about the hamstrings. There’s an inflammatory process, so it swells down in that area. With the swelling and the damage to the tissue comes pain.
You probably did the best thing you could do. You previously ran, and you just said, recently, you got rid of it, and I bet your barbell training has been great for developing the strength of that origin of that tendon. With something like that, the number-one thing we want to do is we can treat that area. There are things we can do. We can do dry needling to that area. We can do e-stim to that area. We can go up and friction massage. We can stretch it. We can do strain and counterstrain work, where we do eccentric dynamic loads on it.
But you know what I would do with a patient that has that? I’ll give you a good example. I had a young football kid that saw me several years back. He played football for a very large high school locally, and he wanted to get rehab for a hamstring tear or sprain and strain that he had had. He had five different hamstring sprains in the last two years as a football player. His brother was already playing at a Division 1 college. He had great genetics, so the goal was to get him back to playing at a level where he could participate in the college combine and hopefully get a good school big to go play football.
His dad brought him to us. One of the other therapists, who’s one of my business partners, was actually treating him, and I just filled in one day for him. I got to talking to the dad, got to know him a little bit, and so we did the rehab on him. The way that we rehabbed him was we had him do good mornings, deadlifts, back squats, weighted lunges. We really worked on developing the tendon strength at its origin at that sit bone through eccentric and concentric weight training. As time went on, his father contacted me and said, “Hey, he wants to get stronger,” so I think it was December a year ago he started strength training with me. I think we started him in the first week of December. He was back squatting 275 for 3 sets of 5. When I finished with him in February, I think he did 3 sets of 5 at 430 on the back squat. I think he was deadlifting close to 500 pounds, and he went and sat for the college combine and got a bid to go play football at a school.
I think the key there is that we’ve got to sometimes give the human body … It’s based on the severity of the injury. In a case like yours, if you had torn that tendon from its origin, if it had been … Do you know the grades of the tears, Brett, the different grades of tears?
Brett McKay: I don’t.
Darin Deaton: A grade one would be a minor tear. There’s really no structural tear to the tendon, where it originates on the bone. It’s just an irritation. There’s an overstretch. A grade two, there’s a very small tear; 0 to 25% of it’s fibers. A grade three, 25, 50% of it’s fibers, up to 75% of it’s fibers. Then a grade four would be a complete rupture of the tendon or just barely hanging on there. If someone came to me and said they felt a pop up in there and it was very painful and they had very poor hamstring strength, very poor hip extension and knee flexion, I want to make sure what we’re dealing with there. I might even get an MRI of that or a CT scan just to figure out what level of tear or injury are we dealing with. Does that make sense?
Brett McKay: No, yeah, that makes sense.
Darin Deaton: But, yeah, I think you did exactly what you should have done. Running doesn’t make you a stronger runner. It makes you have better aerobic capacity, potentially, and your feet are able to handle the pounding better. You get chaffing in the right spots. You’ve got to do some mileage, but I think, also, a stronger runner is a faster runner.
Brett McKay: You mentioned some alternative recovery or rehab tools. It seems like, in the past, I’d say, five years, there’s been more attention paid to rehab and recovery. I remember when I started training in high school, barbell training, it basically was like, if you’re hurt, go sit in the ice bath, and that was it. Now there’s all this stuff. As a practitioner, what stuff actually works, and why does it work? You mentioned dry needling. What is that? Cupping is another one. What do those do, and do those actually do anything? What do they do for rehab and recovery?
Darin Deaton: I’ve got to give away all my secrets and tricks?
Brett McKay: Right, no, just a few of them, right?
Darin Deaton: I can’t give away my snake oil tricks here. No, I think, unfortunately, there’s a lot of things that are being done in clinics today that there is not a lot of research to support some of those things. I try to stick with the ones that I know. In medicine, we use this thing called evidence-based practice, and, little bit, it’s a three-pronged stool. Think of a stool that’s sitting on the ground. It’s got three legs. One of those legs is research, research and data. For most of the physical modalities or treatments that are out there, we still lack the quality of research that we would like to see for support of a lot of those modalities. We have some pretty good data out there, but we still could always use more data.
The second stool leg, the second leg, would be clinical experience, the person that’s actually treating you. What kind of experience and anecdotal and observational evidence do they have as a clinician to say that, hey, I’ve used this on 100 clients and it works? I don’t care if their research supports it or not or if their research is less supportive or minimally supportive. I’ve seen this work.
Then the third one would be the patient value or the client value and the client experience. If a client came into me and said I’ve had ultrasound every single time this has flared up, and ultrasound helps, I’d be remiss if I didn’t use ultrasound, even though I might think that ultrasound’s not going to be as highly as effective as another method, because the patient has built a value in that treatment. Does that make sense?
Brett McKay: Yeah, that makes sense, sure.
Darin Deaton: So if we take that approach, then some of the things that I think that are very effective on an evidence-based model, at varying levels of evidence … Not all these things have the same level of evidence. The number-one thing that we know is the most supported by the literature would be resistance training, even in the physical therapy world. We know that resistance training, using load and weight with set rep schemes … And we would vary that resistance training with three different variables. That would be volume, intensity and frequency. Volume, how much are they going to do of it? Frequency, how often are they going to do it, based on recovery and things like that, based on their injury or, if they’re not a patient, based on their training model? Then, also, intensity, and intensity could be based on the set and rep scheme. It could be based on the load. There’s a lot of things that can vary the intensity, but, generally, that’s the load base of the scheme.
I think resistance training would be the first thing, and a lot of people think that’s old school, and a lot of people think that’s boring. But I think that resistance training is the most effective method for me to rehab clients today. The second thing would be to use my hands. I do joint manipulation on patients sometimes using joint manipulation in the spine and in the extremities. We don’t really know why that works. There’s a lot of theories that are out there, why that works, but I generally get a very good response using joint manipulation with certain types of patients and certain types of diagnoses. We use electrical stimulation, e-stim, in varying forms. Some of it’s contractile-based, where we actually cause a muscle contraction. We’re not trying to get the muscle stronger because that’s a debunked theory, but what we’re trying to do is get good muscle contraction. Then we also might have the patient volitionally … They try to contract the muscle, and then we stimulate the muscle also with muscle stim at the same time, so we’re getting that combined effect. Then we might use e-stim too for pain control or for pain mediation so that they can do more activity and be more active and move more.
Then we use things like dry needling. Dry needling is a great technique. Dry needling is the Western form of acupuncture, and we know acupuncture has good benefits. But as a therapists that’s certified in dry needling, I use dry needling for the physiological effect that it creates, increased blood flow, increased firing of the local receptors in the region, the improvement in reducing trigger point activity and helping the muscle to relax. There’s a dry needling technique that we use on the knee that uses a nine-point technique, where we put needles in nine different locations around the knee. On an osteoarthritic knee, I can put that system on them. I put the nine needles in the knee, combined with a low current electrical stimulation, and they get a great relief in knee pain. We use things like that too.
There’s other things that we could use, and there’s some modalities that are used in the sports medicine world today. Really, there’s very little research to support those things, and I try to stay away from those things.
Brett McKay: I sounds like what the dry needling does, you’re basically creating an inflammation to drive blood there to treat a subline inflammation, right?
Darin Deaton: Yeah, I mean, theoretically, that would be it. We would generally use dry needling when the primary healing model has failed to heal the region. What we’re trying to do, like you said, is we’re trying to create another incident that the body would see as an injury. That incident, what we’re trying to do is influence the body I increase the blood flow. It cases a small inflammatory process that’s more controllable, and then, hopefully, through exercise and activity and education, we can get the patient moving again and get the inflammation down. Inflammation causes pain. Structural damage causes pain. We’re trying to get the inflammation down, get the structural damage to heal, but the best way to get that area to heal is to put that tissue under movement. If it’s a contractile tissue, like muscle tissue … Tendons, we really wouldn’t consider a contractile structure on its own, but it’s part of the contractile element because it’s attached to the muscle. The tendon attaches the muscle to the bone, and the ligaments attach bone-to-bone. In those scenarios, we’re trying to get blood flow to all of those tissues so the human body can heal itself.
Brett McKay: It sounds like the first thing you’re going to do in rehab is continue with resistance training at a different level, probably modify the level or the intensity. Then if that doesn’t work, you might incorporate some of these other practices or these other methodologies.
Darin Deaton: Yeah, and I’d probably combine it together. If the client comes in and they’re having some pain, then I’ll probably do … Now it’s based on the severity of the injury. If the injury requires a period … Let me give you an example. Let’s say someone comes in and they have a postop rotator cuff repair. They ripped their rotator cuff off the bone. It’s just been repaired with three or four anchors. They’re in their postop period. There’s certain precautionary measure that we have to take during that period because here’s a structural integrity issue there that we just have to be careful with so we don’t retear the tendon before it has a chance to purchase into the bone. Does that make sense?
Brett McKay: Yeah, that makes sense.
Darin Deaton: In that scenario, what I’m really doing is I’m trying to give them pain mediation first. So let’s say they come in one day postop, well, the first thing we’re going to do is we’re going to start using gentle, gentle passive range of motion. We’re going to clean the postop wounds up. We’re going to dress them. Then we’re going to use ice and e-stim to increase the blood flow to the area, along with that range of motion, and then give them a home program and send them on their way. As the tendon heals and opportunity allows itself, then we’ll start to load that tendon gradually, over time, through a passive to active assistive, to active range of motion model, and then add resistive range of motion whenever it’s appropriate.
There are times, when you’re talking about fractures or structural integrity issues, where a ligament’s been severely damaged, where we’ve got to be careful with motion. We still want motion, but the motion is going to be controlled in regards to its range and its volume and how much load we’re definitely going to put through it. But with all clients, I’m probably going to combine those modalities and those techniques together. So a good example would be they come in. We do some exercise training with them that day, and then we finish the session with ice, e-stim, whatever else we’re going to use, which we consider an adjunctive modality.
Brett McKay: How do you know when a patient’s … they’re good? Because the healing process, it’s like a muddled bleeding, or it bleeds to moment to moment. Is there a moment where you realize, yeah, you’re good to go. You can just go back to what you were doing before.
Darin Deaton: That sounds like the magical looking glass there or something. I wish I had that exact answer to the exact time. I know at this time and at this minute, you healed. But here’s what I teach our new therapists that come out of the … When the DPTs come out of schools and they come into our practices, one of the things that we’ve actually uploaded into what we call our clinical toolbox for our therapists, it’s an evidence-based compendium of articles and different texts, sections out of books that I’ve read or other therapists have read over the years.
One of them is a pathology text, and what I did was I just copied the pages that pertain to the healing timelines and timeframes for different types of human tissue. Doesn’t it make sense that a tree grows at a certain rate, that certain plants grow at certain rates and certain animals grow at certain rates? Humans grow at certain rates, and they also heal at certain rates. We can generally say that most muscles will heal within two to four weeks, and we’ll be pretty structurally strong, unless it’s a severe tear with a lot of bleeding and there’s a lot of damage to the muscle. But when you’re talking about your average sprain, strain, you’re talking about two to four weeks. When you’re talking about tendons and ligaments, you’re probably talking somewhere around six to eight weeks before it’s healed fairly well and we can load it even more and more and more. When you’re talking about bones, then it’s age-dependent, based on how old the person is, but generally we’re talking about … You know, most people are in a cast for somewhere between three to six weeks, based on the severity of the fracture.
The first thing you want to look at is what tissue am I dealing with here? Let’s take the case that you had where you, most likely, had a small tear or disruption of the origin of the hamstring tendon at the sit bone, when you were running. In that scenario, if you came into my clinic and you could produce a strong contraction but it was painful, then I know how to grade that in regards to damage, and I can give you a general idea how much damage is in there before we even look at an MRI. Now let’s say you produce a very week contraction and it was extremely painful and I thought you had a pretty good pain tolerance. Because a lot of it is neuroscience and pain behavior. Some people are just generally more durable than others, and they tolerate things more.
Let’s say I knew you as a friend or a client, a lifting client. You came in, and I knew this guy’s tough. This guy’s tough as nails. You came in, and you produced a very weak contraction in the hamstrings and it was extremely painful. Then that would give me cause to want to see further diagnostics because I’m thinking this is probably a grade two to a grade three tear or strain and sprain. Does that make sense?
Brett McKay: Yeah, that makes sense.
Darin Deaton: So let’s say you came in, and you could produce no contraction of the muscle. You couldn’t extend the hip or flex the knee very well at all, and you had less localized pain, but just more diffuse pain in the general region. But it wasn’t quite as painful as I would have expected it to be. Now I’m really concerned because the muscle’s not contracting in the manner that it’s supposed to. The muscle’s not functioning, and I’m thinking that my muscle may not be attached. Does that make sense there?
Brett McKay: Yeah.
Darin Deaton: So then, from that standpoint, we’re going to rehab you based on the severity of the injury. In some of these cases, they’re surgical. But once you come into rehab, we look at those timeframes, and a great example would be a postop ACL injury or a rotator cuff injury. We have some general time guidelines that we follow. In some of those injuries, you’re going to find that most physical therapists are very, very conservative on those timelines. Because we’re in the medical industry and there’s approach avoidance and clinician do no harm, physician do no harm model and there’s a lot of medical liability there, we have to be careful. I put on two different hats, one hat as a physical therapists and one hat as a strength coach. Once you can reasonably handle body weight load, then we gradually load you over time. When I feel like you’re competent in your movement, you’re handling loads frequently, then I’ll just send you on your own way and let you train yourself and just follow up with me when needed.
Brett McKay: That’s great. Well, Darin, this has been a great conversation packed with information. Is there anywhere where people go to learn more about what you do?
Darin Deaton: Well, unfortunately, I’m old, so I’m in my 50s, and I’m not quite caught up with the whole social media trend. I’m dysfunctional there, but people can get a hold of me if they’d like to at my Barbell Logic Online Coaching email, which is [email protected], or they can get a hold of me through my rehab email address, which is DLD@RiataTherapy … That’s R-I-A-T-A-Therapy.com. I still have my CrossFit Fort Worth website up. It’s Forth Worth Strength and Conditioning, CrossFit Fort Worth. Hopefully, within two months, I plan to open a small, boutique barbell gym in my local community where I’ll mostly be doing barbell training, but also some conditioning on a need basis, specific need basis. I’d love to hear from guys. If you just have a question, a concern, you need more information, that’s the best place to get a hold of me, in those email addresses.
Brett McKay: Awesome. Darin Deaton, thank you so much for your time. It’s been a pleasure.
Darin Deaton: Thank you, Brett, appreciate it.
Brett McKay: My guest today was Darin Deaton. He is a physical therapist as well as a Starting Strength coach. You can find more information about what he does at Barbell Logic Online Coaching. Also, check out our show notes at AoM.is/Deaton. That’s D-E-A-T-O-N, where you can find links to resources where you can delve deeper into this topic. Well, that wraps up another edition of the Art of Manliness Podcast. For more manly tips and advice, make sure to check out the Art of Manliness website at ArtOfManliness.com. Enjoy the podcast. I’ve gotten something out of it. I appreciate if you’d take a minute or two to give us a review on iTunes Stitcher, helps out a lot. If you’ve done that already, thank you. Please share this show with your friends. That’s how this show grows; it’s word of mouth. As always, thank you for your continued support. Until next time, this is Brett McKay telling you to stay manly.