You probably know someone who’s struggled with a severe addiction to drugs or alcohol. Maybe you’re battling a big addiction right now. Even if you don’t have a severe addiction, you might have a habit that you’re not happy with, like looking at your smartphone or playing video games too much. Whether big or small, these compulsive behaviors share a similar underlying cause: they’re an attempt to assuage pain through pleasure. But as my guest today argues, the problem is that the relentless pursuit of pleasure only leads to more pain.
Her name is Anna Lembke and she’s Chief of Stanford’s Addiction Medicine Clinic and the author of the book Dopamine Nation: Finding Balance in an Age of Indulgence. At the start of our conversation, Anna unpacks the definition of addiction, why she believes it applies equally well to substances like drugs as behaviors like using porn, and how it exists on a spectrum from the serious and severe to the mild and minor. Anna explains why life in our comfortable, pleasure-filled modern society is increasing the problem of addiction, and argues that the reason we’re so miserable is that we’re working so hard to avoid being miserable. She then digs into the science of why we become addicted to substances and behaviors and how it all comes down to our mind and body trying to seek balance between pleasure and pain. We discuss dopamine’s role in this seesaw dynamic and how the substances and technologies of modernity can lead to a dopamine deficit.
We then walk through the process of getting a handle on your addiction, including the importance of doing a dopamine fast, and how long the fast needs to last to be effective. Anna shares tactics for sticking through this abstinence period, which include, counterintuitively, intentionally seeking out pain. She explains why a dopamine fast can help you rebalance your brain, what comes after it’s over, and much more.
Resources Related to the Podcast
- Prohibition Worked Better Than You Think
- What Vietnam Taught Us About Breaking Bad Habits
- Brown and Shuckit’s research on alcohol use and depression
- Nora Volkow’s research on dopamine and addiction
- AoM Podcast #708: Overcoming the Comfort Crisis
- Sunday Fireside: Lash Yourself to the Mast
- Sunday Firesides: Shame Is a Gift
- 4 Lessons From a 4-Week Social Media Fast
Connect with Anna Lembke
Listen to the Podcast! (And don’t forget to leave us a review!)
Listen to the episode on a separate page.
Subscribe to the podcast in the media player of your choice.
Listen ad-free on Stitcher Premium; get a free month when you use code “manliness” at checkout.
Podcast Sponsors
Click here to see a full list of our podcast sponsors.
Read the Transcript!
If you appreciate the full text transcript, please consider donating to AoM. It will help cover the costs of transcription and allow other to enjoy it. Thank you!
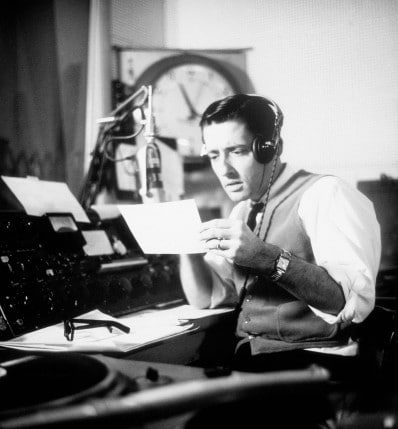
Brett McKay: Brett McKay here, and welcome to another edition of The Art Of Manliness podcast. And you probably know someone who’s struggled with a severe addiction to drugs or alcohol. Maybe you’re battling a big addiction right now. Even if you don’t have a severe addiction that gets in the way of your life, you might have a habit you’re not happy with, like looking at your smartphone or playing video games too much. Whether big or small, these compulsive behaviors share a similar underlying cause, they’re an attempt to assuage pain through pleasure. Plus my guest today argues, the problem is that with limitless pursuit of pleasure, only leads to more pain. Her name is Anna Lembke and she’s Chief of Stanford’s Addiction Medicine Clinic, and the author of the book, Dopamine Nation: Finding Balance In An Age Of Indulgence. At the start of our conversation, Anna unpacks the definition of addiction, why she believes it equally applies to substances like drugs as behaviors like using porn and how it exists on a spectrum from the serious and severe to the mild and minor.
Anna explains why life, and our comfortable, pleasure-filled modern society is increasing the problem of addiction and argues that the reason we’re so miserable, is that we’re working so hard to avoid being miserable. She then digs into the science of why we become addicted to substances and behaviors, and how it all comes down to our mind and body trying to seek balance between pleasure and pain. We discuss dopamine’s role in this see-saw dynamic and how the substances and technologies of modernity can lead to a dopamine deficit. We then walk through the process of getting a handle on your addiction, including the importance of doing a dopamine fast and how long the fast needs to be to be effective. Anna then shares tactics for sticking through this abstinence period, which include counter-intuitively, intentionally seeking out pain. She explains why a dopamine fast can help you re-balance your brain, what comes after it’s over and much more. After the show is over, check at our show notes at aom.is/dopaminenation.
Alright, Anna Lembke welcome to the show.
Anna Lembke: Thank you for having me, I’m excited to be here.
Brett McKay: So you are the medical director of Stanford’s Addiction Medicine Program, and you got a new book out called Dopamine Nation: Finding Balance In The Age Of Indulgence. And this is a… It’s a really easy to follow, easy to understand guide through the science of addiction. And then you also walk readers through the process you use with patients that come to you with addiction problems. So let’s dig into this book. First question, let’s start with definitions. How do you as a clinician define addiction? Because I think a layperson, when they hear the word addiction, they think, “Well, you can be addicted to substances like alcohol or nicotine or cocaine,” but can behaviors be addictions? So yeah, clinically, how do you define addiction?
Anna Lembke: Yeah, so our brains are evolutionarily designed over millions of years to approach pleasure and avoid pain, and anything really that brings us pleasure or gives us relief immediately from pain has the potential to become addictive. Particularly, if we have an innate vulnerability to that problem. Addiction broadly defined is the continued compulsive use of a substance or behavior despite harm to self and/or others. And one way to remember the diagnostic criteria for addiction shorthand is to think of the three Cs, control, compulsion, and consequences. Out of control use, compulsive use, meaning a level of automaticity to the use, and mental preoccupation with using, and then consequences, and especially, the continued use of that substance or behavior despite consequences.
Brett McKay: Alright, so I guess, if there’s not bad consequences, would a substance be able to be considered addictive? Let’s say you have… You just habitually like to, I don’t know, drink orange juice every morning.
Anna Lembke: Right.
Brett McKay: As long as that’s not getting in your way of your life or other’s life that’s not considered an addiction.
Anna Lembke: Absolutely. I mean, this is not to say that anything you enjoy is addictive or even has the potential for addiction, this really is talking about compulsive out-of-control use that is pathological, meaning that it adversely impacts your life and possibly the lives of other people. But I will say that one of the core features of addiction is what we call denial, and as one of my patients said, “Denial is actually an acronym that stands for Don’t Even Know I Am Lying.” So we can be addicted and caught up in an addiction, not see the consequences, even when they’re there.
Brett McKay: So you mentioned behaviors can also be addictive. And I’ve noticed… I’ve kind of kept up with… You see these magazine articles or news stories pop up about the controversy surrounding whether or not a behavior can be considered addictive. So whether shopping… Whether there’s a shopping addiction, Internet addiction, sex addiction. Why has there been so much controversy about whether behaviors can be addictive?
Anna Lembke: You know, I’m not sure. It’s a good question, and you’re absolutely right, there is that controversy there. But in my clinical work, I really see no difference in terms of the natural history of the behaviors, whether the drug is alcohol or whether it’s pornography or whatever it is. People usually start out using their drug for fun or to solve a problem, and that problem can range from depression, anxiety, inability to concentrate, to just plain old boredom. And then if the drug works for them, they naturally repeat use, and over time, they find themselves using every day, or in a binge pattern, in greater and greater quantities, and then ultimately they get to a point where they can’t stop even when they want to. And many patients become depressed and anxious and suicidal, and that is true for a pornography addiction or a gambling addiction, or a gaming addiction, as it is again, for drugs and alcohol. So, I don’t know why there’s this controversy, because I can tell you, I’ve got a front seat to these problems and you can definitely get addicted to behaviors.
Brett McKay: Well, let’s talk about the state of addiction in America today, what’s that like? Are addictive behaviors, addictive substance use, is that on the rise? Do we have an idea how many people have an addiction of some sort?
Anna Lembke: Yeah, so addictions are on the rise all over the world, especially in developed nations. Not only are more people developing addictions, but more people in demographic categories that were previously thought to be immune to addiction are developing addiction, that would include women and older people. It’s also true that more people are dying from their addictions. And if you look at sort of global deaths from addiction, 50% of those deaths are occurring in people under the age of 50. So, we have a lot of young people dying from addiction. I would also add that more and more we’re seeing minor addictions. So, addiction is a spectrum disorder, mild, moderate, and severe, and we’re seeing more and more people with mild addictions, and more and more people with either digital addictions or digitally mediated addiction, so people addicted to their devices, or addicted to a portal that the device gives them access to.
Brett McKay: Whether that could be online shopping, pornography, gambling, etcetera?
Anna Lembke: Yeah, exactly. So starting in the early 2000s, I started seeing more and more patients coming in specifically seeking help for pornography, gambling, and gaming addictions, and almost universally, they reported that the tipping point for them was getting a smartphone, which made access 24/7.
Brett McKay: Well, here’s the question that you might know off the top of your head, is it a gender breakdown on addictions? Is there one gender more likely to be addicted than the other?
Anna Lembke: So historically, men are much more likely to become addicted than women in a ratio that ranges between 5 to 1 and 2 to 1. But depending upon the substance, that’s really changed, especially among millennials. So for example, when it comes to alcohol addiction, millennial women are now as likely as a millennial men to develop an alcohol use disorder. And I would say overall, that’s been the big shift gender-wise, that we’ve seen in the last couple of generations, many, many more women presenting with serious addictions, whereas in previous generations, that was not the case. If you break it down by drug, certainly video game addiction, many more men play video games than women, and many more men than women struggle with video game addiction. That’s also true for pornography addiction, gambling addiction.
Brett McKay: I mean, I think you’ve talked about this in the book, the thing that’s driving is that a lot of this stuff is just… It’s easier to access than ever. Gambling, you can gamble from your computer. Pornography, you can access it from your smartphone, where before you would have to go and move yourself physically to obtain these substances, you no longer have to do that.
Anna Lembke: When we think about the risk factors for addiction, one of the risk factors that’s often underestimated is simple access. If you live in a neighborhood where drugs are available on the street corner, you’re more likely to try them and more likely to get addicted. If you go to a doctor who liberally prescribes Xanax and OxyContin, you’re more likely to be exposed and more likely to get addicted. So, you’re absolutely right, it’s the increased access that has become one of the major risk factors for addiction in the modern world.
Brett McKay: And you make this interesting point that I didn’t know about, about Prohibition. I think typically the way we learn about Prohibition in America is like, well, it was just an over-zealous thing. We amended the Constitution, and it caused the black market and we had gangster fights and whatever, and that was a mistake and that’s why we repealed Prohibition. But you highlight… You know, the research says that actually Prohibition worked to reduce alcohol consumption and it had a long lasting effect even after it was repealed. It was like, wasn’t until the 1950s that alcohol consumption started increasing again in America.
Anna Lembke: That’s right. And Prohibition not only decreased alcohol consumption, it decreased rates of public drunkenness. It decreased alcohol-related liver disease, even in the absence of new treatments for that. So, Prohibition had a positive effect on alcohol consumption and the adverse consequences related to it, and that’s a piece of that history that often gets lost and really does demonstrate a natural experiment in which access to a very addictive intoxicant namely alcohol was decreased and as a result, the harms related to use also decreased.
Brett McKay: So there is an increase in availability to addictive substances or, I guess, we would say portals that can encourage addictive behavior. Besides that, what is… I mean, people go to these things, whether it’s alcohol or pornography, because they feel bad, and they’re trying to assuage that to feel better. What is it about modern life? Because you think, “Well, modern life’s great. We’ve got [0:11:09.3] ____. We’ve got antibiotics.” I mean, yeah, there’s some stuff, we got a pandemic going on, but for most part, life’s great. So why do we feel like we need to turn to substances or behaviors to that can be maladaptive to make us feel better?
Anna Lembke: The way that I understand this and it’s a major premise of the book, is that it’s essentially a mismatch between our primitive brain and our modern ecosystem. I mean, our brains were evolved over millions of years for a world of scarcity, in which we would have to work very hard to obtain even a subsistence level kind of survival needs, food, clothing, shelter are main. We now live in a time when those things are available in a kind of horrific over-abundance, and technology has allowed us to make highly potent drugified versions of all of that. At the same time, our lives have become much more comfortable. So we also seldom have to experience any kind of physical pain unless we get ill or unless we intentionally seek it out. And so, it’s this insulation from pain and this constant ingestion of these highly potent intoxicants in many different forms that essentially our brains can’t tolerate, and as a result, we’ve down-regulated our own dopamine and our own dopamine receptors, and essentially inducing a dopamine deficit state. So, to answer your question, I sort of turn it on its head, the reason that I believe that so many of us are so miserable is because we’re working so hard to avoid being miserable.
Brett McKay: That’s counter-intuitive, ’cause most people would say that’s…
Anna Lembke: Yes. Yeah, and it suggests that the antidote is actually to avoid pleasure and to actively seek out challenging, uncomfortable situations.
Brett McKay: Well, let’s dig into the mechanism of addiction here, and you kind of talked about it a little bit just now, so you make this argument, we’ve been so inundated with pleasure that we basically are desensitized to it, so we had to look for stronger and stronger things to give us pleasure. Walk us through this cycle, like, the role that dopamine plays in the addictive process.
Anna Lembke: Sure. So, one of the most interesting findings in neuroscience in the last 75 years is that the same parts of the brain that process the experience of pleasure, also process the experience of pain, and that pleasure and pain work like a balance. So for example, if I do something pleasurable, like eat a piece of chocolate, I get a little release of dopamine in the brain. Dopamine is a neurotransmitter that’s intimately associated with the experience of pleasure, reward and motivation. And that release of dopamine causes my pleasure pain balance to tip to the side of pleasure, but one of the rules governing that balance is that it wants to preserve what’s called homeostasis, it wants to remain level. So no sooner has that happened, than my brain down regulates my own dopamine transmission and my own dopamine receptors, and I imagine that as these little neuro-adaptation gremlins hopping on the pain side of the balance to bring it level again.
But those gremlins like it on the balance, so they don’t get off when the balance is level, they stay on until the balance is tipped an equal and opposite amount to the side of pain, and that’s what’s called the opponent process mechanism, also known as the come down, the hang over, the after effect. Now, if I wait long enough, those gremlins will hop off, that feeling of wanting a second piece of chocolate will resolve and my balance will be restored to a level balance, but if I continue to eat chocolate over and over and over again, essentially that initial pleasurable response gets weaker and shorter, more gremlins hop on the pain side of the balance, and that after response gets stronger and longer, and ultimately, I end up with enough gremlins on the pain side of the balance to fill this whole room. So, I end up with a brain that is in a dopamine deficit state, and in that state, I don’t really enjoy anything, and I have to keep eating chocolate not to feel good, but just to feel normal, and that’s essentially that long slide into addiction.
Now again, the hypothesis is that if we wait long enough and we abstain for long enough, eventually the gremlins will hop off, but it can take a really long time on the order of weeks to months, or in some cases for severe addiction, even years.
Brett McKay: Well, so yeah, the gremlins hop on, in one way you try to counter that is you just try to increase the amount of pleasure, right? So you might… If you’re using drugs, you’re gonna use a stronger and stronger drug to weigh on that pleasure side, but that’s not gonna work. It’s just gonna make things worse and worse. Or like in those instances like with pornography, you have to start looking for kinkier and kinkier stuff, so you can actually feel a bit of pleasure, but in the long run you’re just… It’s… More of those gremlins, those pain gremlins are gonna pop on the other side of the… This pain pleasure seesaw.
Anna Lembke: That is exactly right. We would essentially go to war with our gremlins and they are gonna win, trust me, whether it takes days or weeks or months or years, eventually, no matter how potent the drug, it eventually stops working, and it puts us into this dopamine deficit state or this balance tilted to the side of pain, where when we’re not using, we’re experiencing the universal symptoms of withdrawal from any addictive substance and that’s irritability, anxiety, insomnia, depression, and cravings, intrusive thoughts of wanting to use even when we’re trying not to.
Brett McKay: And in some cases with substances, it can get so… You become so dependent on it, like you said, you just need it to function, there’s people who have severe alcoholism, they say, I have to have a drink, or else I just can’t do normal things, like, I can’t even… I might even die if I stop drinking all of a sudden.
Anna Lembke: Well, that is factually true. So some withdrawal phenomenon, for example, from alcohol or from benzodiazepines like Xanax can literally be life-threatening that when we stop, that balance slams down to the side of pain, we experience a neurophysiologic storm essentially, and then we can seize and die from that. So… And even in the absence of a life-threatening withdrawal, it’s truly a physical phenomenon that is incredibly painful for people to endure. They will then do anything to get their drug, to get them out of that state.
Brett McKay: And another thing you talk about in the book, another problem we have that makes addiction a bigger problem now than it was, say, 100 years ago, is that the substances we use, they’re a lot stronger, the alcohol stronger, like marijuana, the types of marijuana people are using are a lot stronger than baby boomers were smoking at Woodstock in the ’60s, our digital devices, just a constant flux of dopamine, because there’s all this novelty and there’s a lot of moving images that really activate that, so we have that going against us, so not only are things accessible, the things that elicit the dopamine response are a lot stronger.
Anna Lembke: Yeah, there are so many examples of the way that technology has impacted this progression. So for example, in the 1880s, prior to the invention of the cigarette rolling machine, it was possible to put out about four cigarettes per minute, but the cigarette rolling machine made it possible to produce 20,000 cigarettes per minute, and now we’ve got vape pens and JUUL devices, which are as accessible as a USB port and deliver much higher levels of nicotine and increase blood concentrations of nicotine, much higher than even the average cigarette. And that progression can be seen with opioids, with cannabis, with pornography, you name it, technology has allowed for this. Basically, evolution of drugs to higher and higher potency forms available at the tap of a screen.
Brett McKay: So when someone comes to you with an addiction problem, what’s the thing like… I mean is there a common story, a common thread, like the thing that finally said “I’ve got a problem”? Is there a common… Does everyone have a common story or is everyone different?
Anna Lembke: Everyone’s pretty different. I mean, the natural history of the disease is very common. Again, people start out using for fun or to solve a problem, that problem can range from depression, anxiety, insomnia, to just plain old boredom. Over time, and with repeated use, they need more and more to get the same effect, more potent forms. Eventually they get to a point where they’re using every day and they have difficulty stopping even when they want to, and it’s interfering with their lives. But that moment when people come in asking for help is really different for everybody. For some people, it’s after they’ve lost their jobs, their spouses, their houses, they’re in jail, that’s what it takes for some people. For other people, it’s just that look of profound disappointment on their spouse’s face when the spouse realizes that they’ve been lied to.
Brett McKay: So when someone comes in, you walk them through this process, and you’ve developed this acronym DOPAMINE, because dopamine is the thing that’s driving addiction, to summarize this process. And I’d like to walk through this, I think this is really useful.
Anna Lembke: Great.
Brett McKay: You said the D stands for data. So when a patient comes in and you basically… The first thing you do, you wanna get data from them. So what kind of data are you collecting from your patient who’s got an addiction problem?
Anna Lembke: Just really the facts of their use; how much, how often, in what situations, what brand. The point here is really to just to have a kind of judgment-free conversation about the behaviors. And the reason that this is critical is because knowing what people are using really does give a good indication as to how serious the problem is. For example, if they’re using all day, every day, that would be very concerning no matter what the drug is. But also, and probably more importantly, when we are forced to tell another human being what we’re actually consuming, how much, when, it really makes it real to us in a way that it’s not real when it’s just pinging around in our own heads. So that’s an important first step.
Brett McKay: Yeah, I can see that. I imagine a lot of people with an addiction problem, they don’t even know how much they drink or how much pornography they use, ’cause they never thought about it. But this would actually make them realize, “Oh boy, this is a bigger problem than I think it is, or I think it was.”
Anna Lembke: Right, right, exactly. So for example, we sometimes use this approach called the Timeline Follow-Back method where instead of asking patients, “Well, how much alcohol do you drink in a week?” which is, it’s easy to average things out to a lower number, I instead say, “Well, how much alcohol did you have yesterday? And how about the day before yesterday? And how about the day before that?” and it comes out then to their surprise that, “Well, wow, I’m drinking three or four standard drinks per week, which puts me in the 20 to 30 drinks per week range, which puts me in the one percentile. That’s a lot of alcohol,” and all of a sudden, they’re shocked themselves.
Brett McKay: So the day you’re collecting the data, you’re not being judgmental about it, you just wanna get the facts. The next part is O for DOPAMINE, and that stands for objective. What are you hoping to get there when you talk to your patients?
Anna Lembke: So all behavior, no matter how irrational on the face of it, has some rational reason driving it. So here’s where I’m just trying to understand why the patient uses that drug, what it does for them, what’s the reason that they use it. And that’s just really to just understand their inner life, but also validate for them that they wouldn’t be using it if it didn’t have some positive effect.
Brett McKay: And so this can vary from person to person. You get a lot of great, I would call them case studies, of people who… They started, say, Adderall when they were in high school ’cause they thought they had an attention deficit disorder or they felt they were struggling in school, and that quickly accelerated to stronger and stronger drugs, and they started using it more and more and more, and they’ve just kind of forgot about why they originally started.
Anna Lembke: Yeah, kind of forgot about it, and in that patient example, kind of a crutch, because then the Adderall becomes basically a way to procrastinate, to not develop good study habits, ’cause they know they can just take it when they need it and stay up all night and get stuff done. So it can have this kind of paradoxical effect where we just come to depend on it.
Brett McKay: And it seems like figuring out why you use a substance, that can go a long way in helping resolve the addiction, because then you can figure out, “Well, I can do something else to fill that hole or solve that problem that I’m using the drug or the behavior for.”
Anna Lembke: Absolutely, and then we can also ask ourselves honestly, whether or not the reason that you’re using is really accomplishing our purpose. So for example, I’ll hear lots of patients say that they use cannabis because it makes them more creative, but then when I ask them if they’ve actually created anything under the influence, the answer is almost always no, and then they’re forced to reflect on, “Wow, what’s the disconnect between why I’m using this and its actual effect?”
Brett McKay: Alright, so that’s objective, trying to help the patient figure out why they have the addictive behavior, using addictive substance. The P stands for problem. So what are we trying to figure out here?
Anna Lembke: So this is where we get at the unintended consequences, because by the time folks are in my office, there’s almost always an unintended consequence to their use. Again, just using the cannabis example, they might start out using it to go to sleep or to help with anxiety, but over time, that drug has sort of turned on them, which happens because of the gremlins in neuroadaptation, and it’s not working anymore, or it’s actually causing them to be more anxious and paranoid, or maybe the consequence that is unintended is their spouse doesn’t like it, or it’s interfering with their professional goals. So almost always, there’s something about using that’s not working out great, and it’s important to have them articulate that.
Brett McKay: Actually that can be hard, because as you said, people are often in denial, like they have a hard time seeing those unintended consequences.
Anna Lembke: Yes, exactly, which is why the next letter in the acronym, A for abstinence, is such a key intervention because when we’re in our addiction, we don’t always see the consequences, but when we stop using for a period of time, we can better see true cause and effect.
Brett McKay: We’re gonna take a quick break for a word from our sponsors. And now back to the show. Well, let’s dig into abstinence, or as you call it in the book, you call dopamine fasting. Because I thought this was really interesting, and you spend a lot of time in your book talking about it. And you say that 20 years ago, if someone came to you with anxiety or depression, the first thing you would have done is prescribe them an anti-depressant. But now you recommend that they do this dopamine fast, to try a period where they abstain from their addiction. And I can imagine this is a tough sell with patients because maybe they’re hoping for the anti-depressant because that’s just easy, you take a pill. They don’t wanna abstain ’cause that’s really hard. So why is dopamine fasting an important part of the addiction recovery process? And how long does the dopamine fast have to be to be effective?
Anna Lembke: So abstinence is important for two reasons. The first reason is that abstaining from our drug of choice allows time for the gremlins to hop off of the pain side of the balance, for our dopamine, own dopamine regeneration to occur, and for homeostasis or a level balance to be restored, which is fundamental to being able to enjoy other things, which we’re not able to do when we’re deep in our addiction and when our balance is tilted to the side of pain. But also, as I said, that period of abstinence is really key for seeing true cause and effect, because when we’re using our drug, we usually can’t see the consequences as clearly or at all. Other people can see it, but we can’t see it. But when we stop using for a period of time, get past the initial craving and look back, it’s often a bit of a surreal moment where we’re sort of shocked at how invested we were in obtaining and using our drug and can even have this bizarre experience where we don’t quite recognize ourselves.
You’re right that it’s a hard sell. Many patients don’t come in looking for help with substance use or with addictive behaviors. They’re here for anxiety, depression, insomnia. They’re expecting me to write them a prescription or give them some sort of psychotherapy, and had to be told first pass, “Well, I’d like you to do an experiment and try to abstain from your drug for a month and see what’s underneath.” That’s not exactly a welcome message, but the way that I sell that message, and I found that it’s pretty convincing to people is to basically just talk about the neuroscience, the pleasure-pain balance, what happens to dopamine when we chronically ingest these intoxicating drugs and why it may actually be the cause of our anxiety and depression and not the consequence.
So I hold out to people the idea that if you wanna feel better, one way to do that is to abstain. And I warn them that in the first two weeks, they’re gonna feel worse before they feel better, and this will be the balance tip to the side of pain before the gremlins have time to hop off, but if they can just wait long enough and get through it, they’ll find that at week three and four, the sun starts to come out. I also importantly tell people, “If at week four you’re actually not feeling better, even if you were able to abstain as I asked, then that’s also really useful information, because it tells me that it’s not your consumption of this drug, but it’s an underlying psychiatric disorder other than the drug.”
Brett McKay: Great. So just to catch that there, when you ask a patient to abstain, it’s not just for a week, you’re asking… You’re going like a month, typically?
Anna Lembke: Right. With severe addiction or people with more severe symptoms, I have found that a month is about the minimum amount of time. And if it’s a pornography addiction, then that means no orgasms for a month with themselves or others. If it’s a screen addiction, that means no screens for a month. If it’s alcohol, it’s no alcohol for a month. Again, the caveat there being that that would have to be a person in whom stopping cold turkey would not illicit life-threatening alcohol withdrawal. But assuming that there’s no danger of that, then it would be stopping alcohol for a month. And my clinical experience has shown me, again, that you need a month really to reset dopamine pathways and restore homeostasis.
And there’s also some scientific literature supporting that. There’s a study by Brown and Schuckit, they took men who are addicted to alcohol and also met criteria for a major depressive episode, and put them on a psych ward where they didn’t have access to alcohol, and otherwise gave them no treatment for depression, and after a month, approximately 80% of those individuals no longer met criteria for depression. Which means that most of those individuals, the vast majority had alcohol-induced depression, and once they were able to stop drinking for a month, they felt a lot better. It also means that 20% of them were still depressed in a month and needed treatment for major depression in addition to their treatment for an alcohol addiction.
Likewise, there are studies by Nora Volkow from the National Institute of Drug Abuse, looking at brain scans of people who have stopped using drugs two weeks prior, and comparing those brain scans with healthy controls, and finding that dopamine transmission in people who have been using drugs who stopped two weeks prior, that was still below normal, hadn’t yet made it back up to normal dopamine transmission, suggesting again that two weeks is insufficient and that more time is needed.
Brett McKay: I think it’s an interesting point too to highlight. I’m gonna flesh that a little bit more and bring it to everyone’s attention. By abstaining… So a lot of people, they say they use a substance or they view pornography ’cause they’re depressed. You’re saying that, no, it could be. We have to abstain to find out. It could be you’re depressed and you’re using pornography or using drugs or alcohol to assuage your depression or anxiety.
Anna Lembke: Yeah, so just to clarify, what I’m trying to say is that, that people feel symptoms of depression and anxiety and are using a drug, and they will tell you that the reason that they use that drug is to help with their depression and anxiety. And they will also say that in the moment when they use, they briefly feel better. So of course, it makes sense to them and to me that they feel like the drug is treating their depression and anxiety. But what I posit to them is that in fact, what may be happening is they’re actually medicating withdrawal from the last dose of their drug, and that the use of the drug is the underlying cause of the depression and anxiety and is driving that phenomenon, and is created by this pleasure-pain balance, putting them in a dopamine deficit state to compensate for the huge surge in dopamine they’re getting from the drug. So it’s a little bit… I don’t know if I explain that okay, but it’s…
Brett McKay: No, that makes sense.
Anna Lembke: Okay, yeah. So it’s certainly a little counter-intuitive because subjectively in the moment, it feels like the drugs are helping, but in the long run, it’s really making things worse or even causing the symptoms in the first place.
Brett McKay: So when you’re working with a patient in this one-month-long abstaining process, are there any tactics that you suggest to help them get through that, so when they’re having that week one, week two, and they’re like, “Oh, I really need… ” They have that craving. Anything you suggest that helps them get through that?
Anna Lembke: Yeah, lots of different suggestions. So one of the things I do first is to just reassure them that it’s time-limited, it’s withdrawal-mediated, and if they can just make it through those first couple of weeks, by week three and four, it really does get better. And that alone in my experience is very helpful to patients because they can just wait and endure and know that it’s going to get better. The other thing that I recommend is that they tell the truth during that time period. So often our addictive use is connected with lying, and lying, I have a whole chapter on it, can also be a trigger for relapse. So one of the key things is to try very hard not to lie about their use in the month ahead that they’re trying to abstain, and also not lie about anything, because I’ve found that that helps people maintain abstinence.
And then the other thing that I recommend is that they do something even more counter-intuitive and intentionally press on the pain side of the balance so that they can speed along the process of restoring homeostasis and resetting their dopamine reward pathway, and that’s done by things like exercise, cold water immersion, engaging in intellectually challenging activities, reading a hard non-fiction book, for example, in my case, or engaging in a labor-intensive intellectual creative activity.
Brett McKay: Yeah, I’d like to dig more into the radical honesty and the pressing on the pain, ’cause I thought that was really… It’s counter-intuitive, it’s really interesting. And then also the abstain thing, you also give suggestions on self-binding, kinda taking the Odysseus approach, like finding ways… When Odysseus went to go confront the sirens, finding ways to basically take the addictive substance or behavior, get it out of your environment so you… ‘Cause as we know, when things are accessible you’re more likely to do it. So make it less accessible, you’ll be less likely to use it.
Anna Lembke: Yes, absolutely. So we talk about the ways in which willpower is a finite resource for all humans and it lasts about a day and it wanes toward the end of the day. And so it’s really important to put literal and meta-cognitive barriers between ourselves and our drug of choice to extend our ability to use our willpower to resist the drug. And that comes in many different forms. As you pointed out, getting the drug out of the house. For my patients who travel a lot, and these are all tricks I’ve learned from patients, they’ll call the hotel in advance and ask the hotel to remove the mini bar from the hotel room. I’ve even had patients who ask the hotel to remove the television set from the hotel room so that they’re not inclined to view things that they don’t wanna be viewing while they walked in their hotel room.
Other things are sort of just setting those kinds of barriers. Because the truth is, we live in a very addictogenic world, and it’s hard for any of us to resist when we’re constantly getting triggered and prompted. So we really have to change the environment in order to be able to successfully exercise our self-control.
Brett McKay: I’ve come across that one study about how the environment can influence addictive behaviors. It was like the Vietnam and heroin.
Anna Lembke: Right.
Brett McKay: Right. So yeah, there was… After the Vietnam war was over, I guess the government was really worried that the returning soldiers, I guess they started using… A lot of ’em start using heroin in Vietnam ’cause it’s readily accessible, and of course, they’re under a lot of stress there. And they’re worried, well these guys are gonna come back and they’re still gonna have a heroin addiction. But what they found out was actually, once they came back, they didn’t have that problem anymore ’cause they were out of that environment that encouraged the heroin use, and there was no readily available heroin.
Anna Lembke: Yes, exactly. It’s a nice corollary to the prohibition example, that when people are in an environment of decreased access, they’re less likely to use and they’re less likely to use in an addictive way. And obviously the inverse is true, when you’re flooded with dopaminergic drugs and behaviors, it’s very, very hard to resist. So part of our challenge in modern life is to create these barriers between ourselves and all of the various temptations.
Brett McKay: Alright, so let’s finish up with this dopamine acronyms. So we talked about D-O-P-A, which is abstinence. The next ones are M for mindfulness, I for insight and N for next steps, and then E for experiment. Can you quickly walk us through these like, what are you hoping the patient sees when you walk them through these things?
Anna Lembke: Yeah, so the M for mindfulness just means that in that initial experiment of the dopamine fast or abstinence from our drug, we will experience a lot of psychological distress due to withdrawal. But also due to just having to tolerate a lot of negative feelings without escaping from those into using our drug. And this is hard to do, but also a really good opportunity. For mindfulness defined as observing our thoughts, emotions and experiences without judgment, and so I just really encourage people to be very compassionate with themselves and to be curious about what comes up and to practice the art of mindfulness. And then insight is what often comes with this experiment. Again, as people get distance from their drug of choice, they’re much better able to see true cause and effect.
And that can be a real shocking eye-opener for people when they realize “Wow, I really was addicted, and I didn’t realize until I tried to stop using.” Or “I didn’t realize until I kind of came out of that vortex of compulsive over-consumption and looked back at who I was when I was using.” So it’s an opportunity for insight and for cause and effect. And when folks come back a month later and they were successful in their month of abstinence, then we talk about next steps, which is the N of the dopamine acronym. And next steps is just all about, what do you wanna do next? If they abstained and they were able to do it and it was a good outcome for them, I say then, “Well, do you wanna abstain for another month, or do you wanna go back to using?” And almost universally, people wanna go back to using, but they wanna use differently. They wanna use less, they wanna use in a way that’s more within their control, that they wanna use in a way that’s more consistent with their values. So essentially then we talk again about self-binding strategies and what moderation would look like, and we get very, very specific here because again, the devil is always in the details.
So how many days a week are you gonna use or how many days a month? What exactly are you gonna use? What’s the context in which you’re gonna use? So for example, my patient with video game addiction, he decided he would only play two or three days a week, no more than two hours a day. He would only play with friends and never with strangers, ’cause once he started to play with strangers, he realized he would go down the rabbit hole. Then he decided there were certain video games like League of Legends that he just could never play because they’re too potent for him and he can’t control himself. So it’s that kind of thing. And then the E of the dopamine acronym, just stands for experiment. That’s where the folks then go back out into the world armed with this new homeostasis and a plan for moderation, and they put it to the test.
Brett McKay: So, I wanna circle back to this idea, besides the self-binding techniques to help them when they’re in that abstinence part, you also encourage your patients to… Would you call press on the pain side of this pleasure pain balance seesaw. And you mentioned earlier, this is doing like things that are uncomfortable, so it could be cold water immersion, reading a hard book, doing exercise. What is it about pressing on the pain that helps that rebalance process that we’re trying to get back to a good homeostasis with our pleasure and pain?
Anna Lembke: The reason that pressing on the pain side is useful is because the same opponent process mechanism that leads to neuro adaptation when we ingest intoxicants that press on the pleasure side also can occur when we engage in activities that immediately press on the pain side. So what happens when we do something like exercise, for example, is that those gremlins will adapt by hopping on the pleasure side and with repeated exposure, that pleasure will be longer and stronger. And so we still get access to dopamine, but it’s an indirect source, and therefore is less vulnerable to this problem of tolerance, dependence and withdrawal.
Brett McKay: Gotcha, and so yeah, you highlight one patient who got really into cold water immersion as a way to help him with his recovering from addiction.
Anna Lembke: Yeah, so he sort of serendipitously discovered that these really cold showers gave him a feeling similar to Vicodin and it would last hours. And so he pursued this as part of his early recovery and continued it years later. It was a way for him to get that same feeling, but in a way that was more enduring and ultimately a more manageable for him.
Brett McKay: And then another thing you encourage your patients too, is to be radically honest about their addiction. And I think that you talk about how the Alcoholics Anonymous has figured this out serendipitously. Like that’s part of the process. But then there’s also neuro-biological research that confirms that yeah, there’s something about being honest that helps you be less addicted to the stuff that you’re addicted to.
Anna Lembke: Yeah, so one of the fascinating things about sort of telling the truth, which by the way, is hard, and which all of us have to exert our will to do because we’re all natural liars, even if the lies seem innocent on their face. But honesty has this remarkable ability to basically stimulate our prefrontal cortex, and I think probably strengthen connections between the prefrontal cortex and the lower brainstem reward pathways, because one of the things that happens in addiction is that our reward pathway stops talking and communicating with our prefrontal cortex, which is a fundamental to the problem, because our prefrontal cortex is what allows us to delay gratification, make good choices, narrate our lives, assess future consequences, and when that gets disconnected, then we were less able to manage our impulses and our compulsive, consumptive tendencies. So radical honesty is really a way to manage and be aware of what our reward pathway is doing.
It also has many other potential benefits. It can foster true intimacy, and we do know that social connection, especially deep and honest social connections release dopamine, so it’s a healthy source of dopamine. It also allows us to be more authentic and more connected to our real selves, which is key to being present in the moment and experiencing ourselves as sort of tethered to the world. I think that’s an especially important aspect in this age of social media and curated online selves. When people often exist online with a persona that’s wildly different from their real lives, leading to feelings of derealization and deep personalization that can make people feel anxious and suicidal. So being our true and authentic selves, again, makes us feel more real in the world. And there are many other examples that I give in the book for why telling the truth is really not just good for recovery, but important to a life well lived.
Brett McKay: So another part of the process that you encourage your patients to go through, or you encourage in the process, which is… And again, it’s counter-intuitive, is what I love about your book is all these all these counter-intuitive things, is fostering shame, but healthy shame. This is interesting, ’cause we often… Typically I think in our modern world, we think shame is completely bad. We’d rather feel guilty. So guilt is you feel bad for the thing you did, but you’re not a bad person. Shame is you did something bad, so it says something about you as a person.
Anna Lembke: Right.
Brett McKay: So tell us about this. Like how can we use shame in a healthy way to overcome addictions?
Anna Lembke: Yeah, So I argue that shame is one of the most powerful pro-social emotions, because shame is essentially connected with the fear of abandonment or being kicked out of the tribe for our transgressions against social norms, and we have this idea that we should sort of de-shame everything because the experience of shame is so painful. I mean certainly it’s true that shaming people can contribute to poor outcomes, but it’s also true that shame can be a very important vehicle for positive change, as long as shame is accompanied by a clear pathway for change and reassurance from the group that that individual will not be excluded from the group. And this is where I think Alcoholics Anonymous is such a remarkable organization because they really get shame right.
A lot of patients will report that the immediate experience of joining AA is a de-shaming experience where they realize they’re not the only ones who have this problem, but at the same time that joining AA is de-shaming, it’s also true that many patients will report that one of the big motivators for not drinking or not using is because they would be mortified to go back to their group and say, “I relapsed”, or have to start the steps over again, which is what you have to do in AA if you relapse. And yet at the same time, if they do relapse, they’re welcomed with open arms, and in fact, the relapse itself represents a positive club good… This is a social and a behavioral economics term, but it becomes a club good for the group as a whole, because then there are opportunities, for example, for people to sponsor that individual, which is a giving back or a service. Relapse also becomes part of the extended hippocampus of AA where people are reminded of what relapse looks like and warned against relapsing themselves. So AA has really figured it out how to leverage shame in a positive direction to help people make good behavior change.
Brett McKay: So the shame can be healthy if there’s a possibility for redemption, it’s what it sounds like.
Anna Lembke: Yeah. Yep, if you can redeem yourself within the group, if you’re not shunned, and if your brokenness is in and of itself, of value to the group. Well, it can sometimes happen in strict religious organizations who give lip service to helping people with addiction, but actually end up not helping them, is that when these kinds of problems are discovered and not immediately resolved, then these individuals are essentially shunned because they sort of become bad advertising for the religious organization. The idea being that if you only believed enough you wouldn’t have this problem. And that becomes very problematic for people with a chronic relapsing and remitting problem like addiction, whereas in Alcoholics Anonymous, it’s the chronic relapsing and remitting nature of it that keeps people coming back, and again, which serves as a kind of cautionary tale for other people in the group and a reminder of how bad it can get.
Brett McKay: And what’s great about this process that we just walked through is that this works for… Like you said earlier, addiction is on a spectrum. So you can have big severe addictions or even mild and minor addictions, and this process works for those minor and mild addictions as well. So you could try this, for example, if you feel like you’re checking your phone too much. So you could do a dopamine fast for a month by deleting all the apps that you waste time on from your phone, don’t check those for a month, and then maybe bring that stuff back, but have blockers in place that limit the amount of time you spend on them. So it works for that kind of thing as well, this process, and for people who are interested in learning more, all about this, where could people go to learn more about the book and your work?
Anna Lembke: You know, I’m not on social media.
Brett McKay: That’s good.
Anna Lembke: Yeah. I was asked by my publishers to create a website for the book, so there’s a website annalembke.com but there’s not too much information out there except for the book itself. But it does come in e-book form and in an audible form, so if folks are listeners instead of readers, there’s a way to listen to the book as well as to read it.
Brett McKay: Fantastic. Well, Anna Lembke, thanks for this your time, it’s been a pleasure.
Anna Lembke: My pleasure, thanks for having me.
Brett McKay: My guest, it was Anna Lembke, she’s the author of the book, Dopamine Nation: Finding Balance in the Age of Indulgence. It’s available on amazon.com and book stores everywhere. You can find out more information about her work at her website, annalembke.com. Also check out our show notes at aom.is/dopaminenation where you can find links to resources, where you can delve deeper into this topic.
Well, that wraps up another edition of the AOM podcast. Make sure to check out our Art of Manliness website at artofmanliness.com, where you can find our podcast archives as well as thousands of articles we’ve written over the years about pretty much anything you can think of. And if you’d like to enjoy ad-free episodes of the AOM podcast, you can do so on Stitcher Premium. Head over to stitcherpremium.com, sign up, use code “manliness” at checkout for a free month trial. Once you’re signed-up, download the Stitcher app on Android or iOS, and you start enjoying ad-free episodes of the AOM podcast. And if you haven’t done so already, I’d appreciate if you’d take one minute to give us a review on Apple Podcasts or Stitcher. It helps out a lot, and if you’ve done that already, thank you. Please consider sharing the show with a friend or a family member, if you think they’ll get something out of it. As always, thank you for the continued support. Until next time, this is Brett McKay, reminding you to not only listen to The AOM podcast but put what you’ve heard into action.