Mental illnesses of all kinds are on the rise, and yet we seem no closer to being able to treat them effectively. We’re only able to treat the symptoms of mental illness, but aren’t often able to put the illness into remission because its root cause has been a mystery.
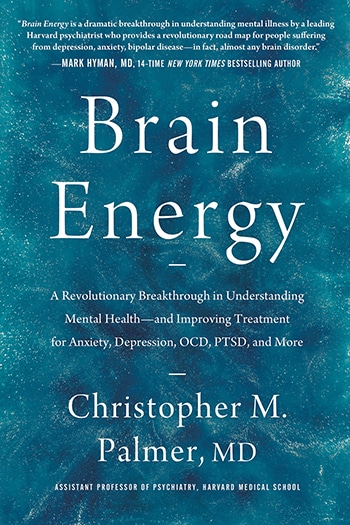
My guest, however, believes he knows exactly what the root cause of mental illness is, and thus how to finally resolve it for good. His name is Dr. Christopher Palmer, and he’s a Harvard psychiatrist and the author of Brain Energy: A Revolutionary Breakthrough in Understanding Mental Health. Today on the show, Chris unpacks his theory of mental illness, which basically comes down to this: if your brain cells aren’t getting enough energy, they’re not going to function properly. He explains how numerous and seemingly diverse mental illnesses, from anxiety and depression to ADHD and alcoholism, actually all have a common pathway: metabolic disorders. While we typically think of metabolism as related to the physical body, it also greatly affects the mind, and Chris explains how you can have the kind of metabolic problems that cause mental illness even if you’re not overweight. Chris then shares how certain lifestyle changes, like switching to a ketogenic diet, may be able to completely cure mental illness.
Resources Related to the Episode
- AoM Podcast #585: Inflammation, Saunas, and the New Science of Depression
- AoM Podcast #793: The New Science of Metabolism and Weight Loss
- AoM Podcast #747: Why We Get Sick
Connect With Dr. Christopher Palmer
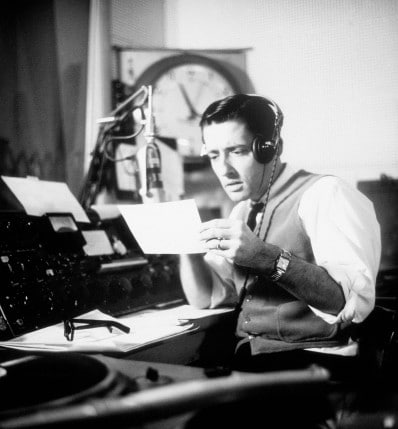
Listen to the Podcast! (And don’t forget to leave us a review!)
Listen to the episode on a separate page.
Subscribe to the podcast in the media player of your choice.
Listen ad-free on Stitcher Premium; get a free month when you use code “manliness” at checkout.
Podcast Sponsors
Click here to see a full list of our podcast sponsors
Read the Transcript
Brett McKay: Brett McKay here and welcome to another edition of the Art of Manliness podcast. Mental illnesses of all kinds are on the rise, yet we seem no closer to being able to treat them effectively. We’re only able to treat the symptoms of mental illness, but aren’t often able to put the illness into remission because its root cause has been a mystery. My guest, however, believes he knows exactly what the root cause of mental illness is and thus how to finally resolve it for good. His name is Dr. Christopher Palmer, he’s a Harvard psychiatrist and the author of Brain Energy: A Revolutionary Breakthrough in Understanding Mental Health. Today on the show, Chris unpacks his theory of mental illness, which basically comes down to this. If your brain cells aren’t getting enough energy, they’re not going to function properly. He explains how numerous and seemingly diverse mental illnesses, from anxiety and depression to ADHD and alcoholism, actually all have a common pathway, metabolic disorders. While we typically think of metabolism as related to the physical body, it also greatly affects the mind. And Chris explains how you can have the kind of metabolic problems that cause mental illness, even if you’re not overweight.
Chris then shares how certain lifestyle changes, like switching to a ketogenic diet, may be able to completely cure mental illness. After the show is over, check out our show notes at aom.is/brainenergy.
All right, Dr. Christopher Palmer, welcome to the show.
Dr. Christopher Palmer: Thank you, Brett, for having me.
Brett McKay: So you are an assistant professor of psychiatry at Harvard Medical School, and you got a new book out called Brain Energy, where you lay out this new theory about a potential underlying cause of all mental illness, depression, anxiety, OCD, even bipolar disorder. It’s really interesting. But before we get into the theory, let’s talk about why treating mental illness has been so difficult. Because, you know, mental health is something society’s been focusing more on. We’re talking more about it, we’re researching it more, you know, millions, billions of dollars have gone into studying it. But more and more people are struggling with mental illness. The numbers keep going up. So why has mental illness been so hard to treat?
Dr. Christopher Palmer: At the end of the day, the real reason is because nobody can say for sure what causes mental illness. All we know are some of the factors involved. We know that neurotransmitters seem to play a role, hormones, genetics, and epigenetics, inflammation, but also psychological and social factors, things like trauma and stress and substance use. And all of these things seem to play a role in mental illness, but nobody knows how they all come together. Nobody knows how they impact the brain to result in what we call mental illness. And so, largely all we have are treatments that were usually discovered through serendipity. So, you know, the first antipsychotic medication was actually being used for anesthesia. The first antidepressant discovered was actually an anti-tuberculosis treatment. And so, these medications were discovered through serendipity and we largely still don’t fully understand how they work or why they decrease symptoms. But for the most part, what is clear is that our treatments only decrease the symptoms. For the most part, we don’t have cures for mental illness. And this even includes things like psychotherapy. So when somebody is suffering from post-traumatic stress disorder or even chronic depression, psychotherapy more often than not does not cure mental illness.
And so, we are largely just scrambling, just throwing any treatments we can think of at people with mental illness. But the sad reality is when you look at the overall treatment outcomes, and I don’t say this lightly, I’m a Harvard psychiatrist, I take this field very seriously and more importantly, I take the suffering of people with mental illness quite seriously. And for people who are getting effective help, that’s great and I’m not here to take anything away from you. If your medications are working for you, that’s fantastic. If psychotherapy has cured you, that’s fantastic. I don’t wanna take any of that away. But for most people with mental illness who get treatment, well over 50% of people who get treatment for mental illness, they do not get remission of illness, meaning their illness is no longer there. And even if they do get a remission, it is almost always short-lived, meaning it can go away for six months or a year or so, but the symptoms are going to come back and you’re gonna have to be changing pills or finding a new psychotherapist or doing something different because your illness is a chronic debilitating illness.
And although that sounds really bleak and abysmal and pessimistic, it is the reality. And for anybody who questions that, the reality is that mental disorders are now the leading cause of disability in the United States and on the planet. And it’s not because people aren’t getting treatment, it’s because our treatments are failing to work. And the number one disabling disorder of all psychiatric disorders, it’s not schizophrenia, it’s not bipolar, it’s plain old simple depression. Depression disables more human beings than any medical illness, including heart failure, cancer, back pain, all physical disorders. Depression disables more people than anything else on the planet.
Brett McKay: Yeah. And as you said, when people treat mental illness, basically there’s two, I guess in the history of mental health, there is two approaches. There’s a physiological approach and then there’s the psychological, so like the mind-body. And so the body part is like, “Well, you know, what’s going on is your brain, it’s not making enough neurotransmitters. So we’ll give you a drug that will help.” And that helps some people, right? ‘Cause maybe that is a symptom. They have lower serotonin, for example, maybe. Maybe we don’t know. But then there’s another field that can say, “Well, no, it’s not a body or physiological thing. It’s a psychological… Your mind, it’s got maladaptive thoughts. So if you do talk therapy, that will help”. Well, it helps some people and that’s the thing. It’s like it’s hit or miss. It’s like, you know, the medication might help someone, but not help another person. And then talk therapy might help somebody, but not the other person. And it’s because there’s… Doctors are just having to figure out, well, what’s the symptom that we need to reduce. You’re not actually treating the underlying cause. You’re just trying to reduce symptoms. So people have a functioning life.
Dr. Christopher Palmer: Absolutely. I mean, I think most mental health clinicians who are treating patients are desperately hoping to treat the underlying cause. You know, I think the mental health clinicians who are prescribing pills are hoping to address that chemical imbalance. And I think the psychotherapists who are delivering psychotherapy are hoping to, you know, relieve the trauma in that person so that the person can let go of their trauma and move on with their life. But again, when we look at the treatment outcome studies, even with the best of intentions, even with the best efforts from all of these clinicians, I’m not here to fault any of them. I, you know, I’m one of them. We’re all doing our best, but our current model of mental health and mental illness and how to treat it is failing miserably.
Brett McKay: And the other problem with mental illness is there’s no objective criteria, right? There’s not like an MRI scan where you can look on someone’s brain who comes in with depression and say, “Yeah, you’ve got depression.” I mean, there’s been some studies saying that, you know, parts of the brain might light up less if you have depression, but there’s nothing definitive about it. Or there’s not a blood test you could take and say, “Yeah, you’ve got OCD.” And so it’s really, you have to talk to the patient and it’s like, there’s subjective things in there and you can’t downplay the subjective because if someone feels awful, you have to take them on their word. But it gets tricky ’cause like you’re trying to, a doctor is trying to figure out, “Well, he says this, if we do this, will it change the outcome?” So that’s the other hard thing. There’s no definitive test for mental illness, unlike cancer where you can look and say, “Well, you got a tumor or there’s a blood test and we still see the cancer there.”
Dr. Christopher Palmer: Absolutely. And it’s really interesting because if there is a definitive abnormality identified, it’s no longer considered a mental illness. So, for example, people with cancer often have mental symptoms. They often can get severely depressed and fatigued. They can have concentration difficulties. They can even have symptoms consistent with, like cognitive impairment, even so far as dementia. They can get delirious where they’re hallucinating or delusional. And we don’t call that a mental illness because we know that they have cancer and they’re getting cancer treatment and both cancer and its treatments can sometimes cause those symptoms. So in those cases, we don’t call it mental illness. And so the sad reality is that the people for whom we can’t identify an objective cause, we put them in the category of mental disorders.
Brett McKay: So the goal is if we could find an underlying common pathway for mental illness, this would allow us… Treatment could be more effective, right? ‘Cause you could find the underlying thing and let’s start getting into your theory here. The first connection I’d like to make is that one thing you note for potential underlying pathway for mental illness is that mental illnesses, depression, anxiety, OCD, bipolar, they all… There’s some overlap there. What do you mean by that? What are some examples of overlap with mental illness?
Dr. Christopher Palmer: So you know, on the surface, you know, DSM makes sense. So DSM describes different diagnostic categories: OCD, depression, schizophrenia, alcohol use disorder or alcoholism and anorexia nervosa. Most people know what those things mean and they paint very different pictures of the types of people that have those disorders, the symptoms that those people are having and the treatments that might be effective for those people. And so on the surface, DSM makes sense. But when you actually look at real people who have mental illness, first and foremost, it turns out that most people have more than one. Certainly most people who are getting treatment do. So on average, one study found that people getting treatment for mental health had three and a half different diagnoses. So right there, we start to see some breakdown in these diagnostic distinctions. So, for example, you could have schizophrenia or anorexia, but if I look at a group of people with schizophrenia, they’re much, much more likely to also have depression on top of their schizophrenia. They’re also more likely to have anxiety on top of their schizophrenia. And wait, I thought those were different disorders with different causes. Now, a lot of people think, “Well, if you were schizophrenic, wouldn’t you be depressed and anxious?”
But it’s not so simple ’cause it turns out that people with depression and anxiety are actually more likely to go on to develop schizophrenia too. But if I look at a group of people with anorexia, they’re also more likely to be depressed and anxious. And you’re like, “Well, yeah, I guess that makes sense too.” But wait, I thought these were all different disorders and now I’m looking at these different people and clearly the schizophrenic person is having hallucinations and delusions and the person with anorexia is starving herself or himself. So those are clear differences, but a lot of the other symptoms and comorbid diagnoses start to overlap. I think much, much more important is that when we look at root causes for mental illness, because we do know some, genetics is a clear example. We have identified some high-risk genes for mental illness. And most people think, well, you know, they must be specific to specific disorders. Like there must be some schizophrenia genes and some bipolar genes and some depression genes and some anorexia genes. But in fact, that’s not true at all. And we know this, we’ve had the human genome mapped for over 20 years.
The top researchers have been on this. We have had artificial intelligence on the job. We know with certainty there is not one gene in the whole human genome that confers risk for any one specific mental disorder. Instead, one gene confers risks for lots of different mental disorders. So one gene might confer risk for schizophrenia and depression and bipolar disorder and alcoholism and epilepsy and cognitive impairment. So when we look at a root cause like that, it starts to, you know, the diagnoses really start to overlap a lot. And when you start to look at all of that kind of scientific data and all of the research that we have, it turns out that mental illnesses are actually not that distinct from each other after all, even though the symptoms can be wildly different. I’m not here to say that psychosis is the same thing as depression. Those represent different areas of the brain malfunctioning, or they represent different degrees of malfunction in the brain, but they are actually not as distinct as most people believe.
Brett McKay: Okay. So let’s get into the theory in brain energy. And so this idea that all these mental illnesses they have… There’s something in common there, there’s overlap. So suggest that there’s some underlying thing that’s causing all of them. And the argument you’re making is that that thing could be metabolic ill health. And now we’re gonna dig into the details of how this works. I think it’s really interesting. But first you point out this idea that metabolism and mental illness are connected. This isn’t a new idea. Other scientists have, you know, decades ago, have kinda made that suggestion. How did they make that connection? Like where does that connection come from? That, “Okay, if you have depression, then you have something wrong with your metabolism.” How did that connection happen?
Dr. Christopher Palmer: So interestingly, those connections go back centuries. So in the 1800s, it was well documented that diabetes and insanity run in the same families. And insanity was the term they used for what we would now call schizophrenia and bipolar disorder largely. But the researchers noticed that in one family, there seems to be a much higher likelihood of both diabetes and psychotic symptoms. And it goes both ways. So if you have somebody with psychosis and they have children, those children are more likely to go on to develop diabetes, but… Vice versa. If you have somebody with diabetes and they have children, those children are more likely to not only develop diabetes, but also develop a psychotic disorder. Beginning in the 1940s, we have had an accumulating and growing body of evidence that there are metabolic abnormalities in the brains and bodies of people with mental disorders, especially the chronic serious mental disorders.
But it goes across the board, depression, anxiety, PTSD, all the way to bipolar and schizophrenia. You know, we’ve done all of these brain imaging studies, PET scans, SPECT scans, functional MRI. Guess what those scans are measuring? They’re measuring brain metabolism. So all of those studies are showing differences in metabolism. And cutting edge research over the last 20 years has gotten much more specific and granular all the way down to genes, specific risk genes, all the way down to the cellular level, identifying innumerable metabolic problems in people with mental illness.
Brett McKay: So yeah, just to refresh, your metabolism is just your body’s way of using energy or taking food and converting it into energy. And I think people typically, when they think about metabolism, they think about things like diabetes ’cause your insulin is not working right or your cells aren’t responsive to insulin or obesity. If you have a problem with obesity, something’s wrong with your metabolism where it’s storing more fat than using the energy. But a point you make is that the big metabolic conditions we typically think of like diabetes, obesity, even cardiovascular problems. If you look at these people who are getting treated for those issues, oftentimes they have… There’s mental health issues going on there, depression, anxiety, some other serious ones. And it’s correlation. So people would say, “Well, of course, someone who had a heart attack’s gonna be depressed. You had a heart attack,” but you say, well, you’re saying, well, hold on here. Well, maybe there’s something else going on there. Maybe there’s an under, like there’s a connection beyond just having a heart attack, but maybe the heart attack and the depression has an underlying cause and it’s that metabolism.”
Dr. Christopher Palmer: Absolutely. And we have an abundance of evidence. This is not speculation at all. We have decades of research looking at the connection, for instance, between heart attacks and depression. As you said, on the surface, a lot of people are like, “Well, if you had a heart attack, wouldn’t you be depressed?” And as intuitive as that seems, the relationship actually goes the other way too. People with depression are twice as likely to have heart attacks and people with all chronic, all mental disorders, all of them across the board, whether they’re chronic or not, all mental disorders, on average, they die early deaths. On average, men are losing 10 years of life. Women are losing seven years of life. And guess what they’re all dying of the primary number one cause of death in the mentally ill across the board, whether you’ve got anxiety, ADHD, schizophrenia, bipolar, alcoholism, the number one cause of death is heart attacks, but in the mentally ill, they are occurring almost a decade earlier on average.
Brett McKay: So I think a lot of people will not be thinking this is how does metabolism affect your mental health? ‘Cause I think most people think metabolism, they think, well, diabetes, blood sugar, weight gain. So how does the metabolism affect your brain? What’s going on there?
Dr. Christopher Palmer: So at the end of the day, metabolism, you know, is, as you said, it’s about taking food and oxygen and turning it into energy or building blocks that get used to maintain or grow cells and energy and building blocks are essential to the function of all cells. And that includes brain cells. If your brain cells are not getting enough energy or they aren’t getting enough nutrients, guess what? They aren’t going to function properly. And at the end of the day, that is the easiest, simplest way to… I can explain my theory is that if your brain cells aren’t getting enough energy, they aren’t going to function properly. And that malfunction can paradoxically be one of two things. Cells can actually become under-active, but cells can also become overactive or something we call hyper excitable. And those two states kind of under activity of a cell or over activity or hyper excitability of a cell can result in all of the symptoms, all of them that we call symptoms of mental illness. So that is the easiest way for us to understand symptoms of depression or post traumatic stress disorder or even schizophrenia.
Brett McKay: What I love about you doing this book, you kind of walk people through is how metabolism affects these different underlying causes of what we typically think of mental illness. So, for example, neurotransmitters, right? Like, you know, there’s something off with your dopamine or serotonin, but you point out research that metabolism plays a role in our neurotransmitters. How does this metabolism affect our neurotransmitters?
Dr. Christopher Palmer: So at the end of the day, you know, when metabolism is extraordinarily complicated and in order to really start to understand what controls metabolism or what it means to have a metabolic malfunction, you actually have to start to go to this other level of the cell in these tiny little things in most of our cells called mitochondria. And mitochondria actually help us understand the connections between metabolism and brain function. So to answer your specific question, what does metabolism have to do with neurotransmitters? I’m going to focus on metabolism, but more importantly on mitochondria, which are these master regulators of metabolism.
And it turns out that mitochondria are instrumental in producing the building blocks that make neurotransmitters. So they produce the building blocks and the energy required to make serotonin and dopamine and norepinephrine and GABA and acetylcholine and other neurotransmitters. But they also are directly involved in the release and the regulation of these neurotransmitters. And when researchers take mitochondria out of a cell, but kind of infuse, artificially infuse energy or ATP into that cell, the neurotransmitters actually do not get released. So it turns out that mitochondria are playing a critical role, not just in metabolism, but in brain function broadly.
Brett McKay: Gotcha. Okay. So the mitochondria can be off in that it’s not producing enough energy, right? Or it’s producing too much. So like the hyperexcitability would be something like bipolar disorder when you’re having a manic phase, like the cells, your mitochondria is probably producing too much energy for the cells in your brain. And example of it being not enough would be like depression. Is that right?
Dr. Christopher Palmer: It starts to get to it. So hypomania or mania is the one clear example of the brain actually producing too much energy broadly. Almost every other disorder is actually not producing enough energy. And one of the paradoxes of this theory based on rigorous science and decades of clinical observation, one of the paradoxes is that when a cell is energy deprived, it can actually become overactive, which is counterintuitive. But cells have kind of an on cycle and they have an off cycle. They get turned on, but they also get turned off. And energy is required to do both of those things. So cells needing energy to get turned on, that kind of makes sense to most people. Most people will get that. But one of the paradoxes is that once a cell gets turned on, it actually has to have enough energy to turn itself off. And that is a paradox because that can result. So a cell can get turned on and be on very weakly. Maybe it’s only really operating at 60% capacity, but it may not have enough energy to fully turn itself off. And that results in hyperexcitability, which can result in some of the symptoms of mental illness.
Brett McKay: We’re going to take a quick break for a word from our sponsors.
And now back to the show. So sometimes brain cells don’t get enough energy and paradoxically, this means that they can’t turn off, which leads to them being to have hyperexcitability. And then hyperexcitability can lead to mental illness. Do we know what it is about the hyperexcitability of brain cells that causes something like depression? Because like depression, you think, “Well, there’s low energy.” So what’s going on there?
Dr. Christopher Palmer: Yeah, it’s a great question. Hyper-excitable means that that cell is doing something in an exaggerated way, or it’s doing something at the wrong time when it really shouldn’t be doing that. So let me give you an easy example that I use in the book. And that is pain. So pain is a normal human sensation. We all experience it whenever we injure ourselves. But people who have pain disorders have hyper excitable pain nerves or hyper excitable pain systems in their brain. And what that means is that they experience pain for no good reason. Or if they just twist or turn the wrong way, they can experience excruciating pain and that pain can go on for minutes or hours even. It just doesn’t stop. All of those are representations of a hyper-excitable pain system. So when we think about something like depression, depression is actually hardwired into the human brain. It is a normal human emotion. And it is hardwired in our brains. It’s actually hardwired in the brains of many other animals like rats and mice. And those serve as models for researchers who are trying to understand depression. So like pain, depression is a normal thing.
But when it gets turned on for no reason or when it fails to stop or when it kind of gets going in an exaggerated way, those can all be reflections of a hyper-excitable depression kind of pathway or depression system in the human brain. And so what that means is that if your depression systems or networks are hyper-excitable, that is somebody who will experience depression for no good reason and/or they might experience depression for a clear reason. Maybe somebody was mean to them or somebody scolded them, but they have a hyper kind of exaggerated response that they get super depressed and it lasts for days or hours. Whereas most people would move on and be able to be okay with that.
Brett McKay: Okay. So a metabolic ill health can cause a neurotransmitter imbalance. And also another thing that psychologists and psychiatrists know that influence mental illness are hormones, cortisol, thyroid hormone, testosterone, estrogen, but that’s also driven by metabolism, correct?
Dr. Christopher Palmer: Absolutely. Yeah. So one of the things that is so wonderful about this theory is that it connects all of the dots that we know in the mental health field. So it turns out that, you know, mitochondria again play an instrumental role in the production of key hormones like cortisol, estrogen, and testosterone, but a hormone like thyroid hormone, like you mentioned, actually plays a critical role in metabolism and the function of mitochondria. Even a hormone like insulin, which most people think of as a diabetes thing, it turns out insulin is actually located throughout the brain and plays a powerful role in the way your brain functions and also plays a powerful role in brain metabolism.
Brett McKay: Okay. So we would have with insulin, like how does it influence mental illness or mental health? Do we know that?
Dr. Christopher Palmer: We do. So we have, again, so that’s probably one of the clearest connections that goes back to the 1800s this connection between diabetes and mental illness. We know that people with type 2 diabetes or even type 1 diabetes are much more likely to develop mental disorders and pretty much all of them across the board, depression, PTSD, substance use disorders, but also bipolar and schizophrenia. You know, over the last 20 years, we have neuroimaging research showing that people with bipolar disorder and schizophrenia have abnormalities in insulin signaling in their brain.
Brett McKay: Here’s a very clear study that I just want to share with people that really drills this home for everybody and why this matters. You know, one study looked at 5000 kids and followed them from the ages of 1-24. And they found that the kids who had the highest levels of insulin resistance beginning at age 9 were five times more likely, that’s 500% more likely to develop bipolar disorder or schizophrenia or be at risk for those disorders. 500% more likely. That is not trivial. And that kind of information gives us clear strategies to possibly prevent mental illness in young people. It also gives us, you know, lots of treatment options as well.
Well another cause or symptom that mental health practitioners have been treating in recent years to decrease mental illness symptoms is inflammation. So there’s been research showing that people with, you know, major depression, for example, are some of them are highly inflamed and inflammation goes back to metabolism. Correct?
Dr. Christopher Palmer: Absolutely. So metabolism influences inflammation and inflammation influences metabolism. Now, you know, everybody’s heard inflammation. That’s the cause of everything that ails us these days. And yes, in fact, people with mental disorders are more likely on average to have higher levels of inflammation. But I’m here to argue that inflammation in and of itself is neither necessary nor sufficient. Meaning inflammation can’t explain all mental illness and not all people with mental illness even have higher levels of inflammation, at least not that we can measure. So inflammation is an important factor. It clearly plays a role for some people, but I don’t think in and of itself, it is the key. Instead, we have to rise above that and see the broader connections through what we call metabolism in mitochondria.
Brett McKay: Okay. So I think people are seeing here now that metabolism, it underlies a lot of these things. It connects a lot of these things that we often treat as disparate things. So let’s talk about like, I mean, what are the things that mess up our metabolism? And then maybe we can walk through some of these things and how you’ve used, you know, diet or exercise or reducing stress to not only fix people’s metabolism, which can help their diabetes or obesity or cardiovascular, but it also fixes or can treat the mental illness. So let’s talk about diet, for example. How does our diet mess up our metabolism and in turn can cause mental illness?
Dr. Christopher Palmer: Yeah. So I think everybody knows if you eat a bad diet, you’re more likely to become obese or diabetic. So I think most people intuitively know a bad diet can mess up metabolism. What I think most people probably don’t know is that a bad diet can also lead to higher rates of mental illness. So I just mentioned that study in kids. So a bad diet can lead to insulin resistance, which can then go on to lead to much higher rates of bipolar disorder and schizophrenia, but much, much more common are depression and anxiety disorders and other types of disorders. So a bad diet can do all of those things. And what do I mean when I say a bad diet? I mean a diet that causes metabolic dysfunction. So a diet that causes higher levels of inflammation or a diet that impairs hormonal status or a diet that impairs mitochondrial function. And you’re probably wondering, “Well, what the hell are you talking about Chris Palmer? Like what does that mean? What is a bad diet?” Well, a bad diet can include a lot of highly processed foods that are high in sugar, high in fat.
That’s kind of the deadly combination is that sweet spot, lots of sugar and lots of fat. That is not a good diet for any human being on the planet or animal on the planet for that matter. But you know, unfortunately we have added all sorts of chemicals and processed things. You know, I outlined some of the literature on trans-fatty acids. Those actually are really horrible for physical health, like heart attacks, but they’re also really horrible for mental health. Trans-fatty acids have been found to result in higher rates of depression, irritability, even Alzheimer’s disease in people. So again, so mental symptoms and so clearly our diet, you know, it’s not rocket science in a way. I think everybody understands what you eat can affect your heart, like in a very clear and concrete way, like what you eat can actually clog up the arteries of your heart and result in a heart attack. On some level, it’s kind of a no brainer to just understand that what you eat can also affect your brain. If it’s affecting your heart, it’s probably affecting more than just your heart. It’s going throughout your body and the brain happens to be connected to everything.
And the brain is actually one of the more energy consuming organs. And so a lot of what you eat, a lot of those calories and substrates and all the breakdown products, a lot of that’s going up to your brain to fuel your brain cells.
Brett McKay: Well, another thing you point out in this, the diet section of how what we eat can influence our mental health or it would ’cause it’s influencing our metabolism is that doctors have known for a long time that if you want to treat epilepsy, one thing you can do is do fasting or like a ketogenic diet, right? There’s something about a ketogenic diet that reduces epilepsy symptoms, particularly in children. They know this with kids. And, again, that shows like, well, there’s a metabolic thing going on there, right?
Dr. Christopher Palmer: Absolutely. To drill some of this home and make it like real for people to help them understand. It might actually be helpful to share a story if I may.
Brett McKay: Yeah, sure. That’d be great.
Dr. Christopher Palmer: You know, I think most people understand that if you eat a healthy diet, it might help depression or anxiety or even ADHD symptoms. I think most people get that. But what I’m saying is that diet, especially a dietary intervention like the ketogenic diet can actually impact what most people think is an incurable chronic mental disorder. So you mentioned we have decades of research showing that the ketogenic diet, for instance, can stop seizures. That’s a real thing. Seizures are real and people can actually die from them. And so doing a specific type of a diet like the ketogenic diet can actually stop seizures. But the work that I’ve been doing over the last six years is using the ketogenic diet in people with chronic serious mental illness. And so the story that I’ll share with you is a woman, I used a different name. I used fake names for everybody in the book, but she actually gave me permission to use her real name. So in this interview, I’m going to use her real name. Her real name is Doris. Doris was diagnosed with schizophrenia when she was 17 years old. She had daily hallucinations and delusions.
Over the ensuing decades, she tried numerous antipsychotic and mood stabilizing medications, but none of them worked to stop her symptoms. They did cause her to gain a lot of weight. Doris was tormented by her illness. And between the ages of 68 and 70, she tried to kill herself at least six times. When she turned 70, her doctor referred her to a weight loss clinic at Duke University where they were using the ketogenic diet, and for whatever reason, she decided to give it a try. Within two weeks, not only did she start losing weight, but her hallucinations and delusions started going away. Within months, all of her symptoms of schizophrenia were in full and complete remission. Within six months, she was off all her psychiatric medications and remained in full and complete remission. Doris went on to live for another 15 years, medication free, symptom free, out of hospitals, no more psychiatrists or psychologists, no more suicide attempts. When I last spoke with Doris, she said she was happy to be alive. And she actually asked me, pleaded with me to share her story with anyone who would listen in the hopes that her story might help even one other human being.
Sadly, Doris passed away this past January at the age of 85 of COVID pneumonia. I want to let people know Doris is not alone. I now have dozens of cases of similar patients achieving seemingly miraculous recoveries from what we currently think of as chronic mental disorders. There are clinical trials underway, at least five controlled clinical trials, some of the leading psychiatrists and neuroscientists are hot on this trail, but I’m passionate about making these treatments and this theory and this information available to people now because people want help now.
Brett McKay: That’s really powerful. So a perfect example, you treat a metabolic condition, you treat the mental illness, and that was just the diet intervention, changing to a ketogenic diet. And that’s again to say, ketogenic might not be for everybody. I don’t think you want to give the impressions like, “Well, if you have depression, go on a keto diet. It’ll cure your depression.” Maybe, but that’s something you have to talk to a psychiatrist or psychologist about. So we’ve been talking about how mental illness may be caused by metabolic problems and how these metabolic problems can be caused by things like poor diet and things like that. And I think when most people think about metabolic problems, we associate them with things like obesity and diabetes, as we discussed, but we probably all know people who are, they got a healthy weight, they seem to eat a healthy diet, but still deal with things like depression. So what’s going on there? If mental illness is possibly caused by metabolic problems, why are there some people who don’t have the typical metabolic problem markers, nonetheless experience mental health issues?
Dr. Christopher Palmer: So the first thing that I want to clarify in this person that you’re saying is depressed, is I want to understand, is this a normal depression or is this a depression disorder? And so in the way that I described pain and hyper excitability, same deal goes for depression. So depression can be a normal response to adversity. So if a kid is getting bullied and teased relentlessly, or if somebody just got dumped by the love of their life, they are going to be depressed. That is all normal. They do not have a brain disorder. They are having normal reactions to adversity. It doesn’t mean they don’t need help. I think a lot of those people do need help, but the help is obvious and common sense. It is human compassion and support, whether that is through friends, family, whether it’s through a psychotherapist, really doesn’t matter to me, but that person needs compassion and support because they are experiencing adversity in their life. If we’re talking about somebody who has depression for no good reason, or that depression is really exaggerated and unrelenting, then I’m going to say that person does have a brain disorder and that that brain disorder is due to a metabolic problem in their brain.
And I’m really glad you brought up this point about, “Well, doesn’t a metabolic problem mean people are fat and diabetic?” Well, people who are overweight or obese do, on average, tend to be more metabolically unhealthy. And certainly people with diabetes, type 2 diabetes, are more metabolically unhealthy. But there are many other causes of metabolic problems in the human body. So let me give you a clear example that will hopefully kind of help people understand this. So one of the other causes of metabolic problems are toxins, things that are toxic to these things in our cells called mitochondria. And they cause, any toxin will cause metabolic problems. And one clear, easy to understand example is smoking cigarettes. So smoking cigarettes is actually associated with weight loss. On average, people who smoke cigarettes weigh less than people who don’t smoke cigarettes. So this is not a weight issue anymore. This is a smoking issue. And yet, we know with certainty based on decades of research, people who smoke cigarettes are more likely to have heart attacks and strokes. Those are metabolic disorders. They’re also, interestingly, more likely to have insulin resistance and develop type 2 diabetes. Even though most people think of insulin resistance and type 2 diabetes as being related to weight or obesity, smokers, even though they’re thin, tend to develop higher rates of insulin resistance and diabetes.
But guess what else smokers are more likely to develop? Depression. So one study actually followed over 14,000 Korean adults over several years, and they measured whether they were smokers, and/or whether they were depressed. And the people who were not depressed, but they were smokers, were much, much more likely to go on to develop depression in the subsequent years. However, the reverse association was not found. So people who were depressed were not necessarily more likely to go on to become smokers. And so the researchers in that study concluded that smoking seems to cause or contribute to an increased risk for the development of depression. So if I summarize all of that, one metabolic toxin, smoking cigarettes, results in higher rates of cardiovascular disease, insulin resistance, type 2 diabetes, and depression, even though smokers weigh less. So we need to stop thinking about metabolic problems as a weight issue because it is much more than just weight.
Brett McKay: Well, another toxin, obvious one, would be alcohol as well, right?
Dr. Christopher Palmer: Absolutely. And believe it or not, people who drink high amounts of alcohol are more likely to what? Have heart attacks. They’re also more likely to develop type 2 diabetes, interestingly. They’re more likely to develop mental disorders, including depression. So again, one metabolic toxin, alcohol, we know with certainty based on decades of research is a mitochondrial poison, and that is poisoning your metabolism, and that can result in both mental and metabolic disorders.
Brett McKay: And then other things too you talk about in the book that could affect metabolism, but you might not see someone with the obvious signs that they have a metabolic issue like weight gain, if you’re lonely, right? I think there’s studies that show that your likelihood of cardiac problems goes up, insulin resistance also goes up, and that can cause things like depression as well.
Dr. Christopher Palmer: Absolutely. So everybody knows that loneliness could be associated with depression, that just kind of makes sense, and that’s usually what people think. But loneliness, as you mentioned, also results in higher rates of metabolic disorders, heart attacks, strokes, and actually premature death. And so that is one of the major themes of brain energy, is that mental and metabolic are interchangeable and closely related and interconnected. That we can’t talk about mental symptoms or mental disorders without talking about metabolic, but we also can’t talk about metabolic disorders like heart attacks or even obesity without thinking about mental symptoms and mental disorders.
Brett McKay: Okay. So even if you’re not overweight, you can still have metabolic problems because there are metabolic disruptors that don’t show up in weight gain. Things like smoking and drinking can damage your metabolism. Something else that can damage your metabolism is stress and lack of sleep. A lack of exercise can damage your metabolism. And that’s why exercise can improve mental health. So a bunch of things beyond diet can affect metabolism. And that in turn can affect your mental health. How do you imagine this brain energy theory of mental health will change how doctors diagnose and treat people with mental illness? Right now, most people, if they go to a psychiatrist, they’re like, “Man, I’ve got OCD or severe depression.” The typical thing is, “Well, we’ll maybe do some talk therapy, do a pill.” With this brain energy approach, kind of walk us through, like, let’s say someone walks into you and says, “Man, I’ve potentially got major depression,” what would you do?
Dr. Christopher Palmer: I would actually want to do a comprehensive assessment of all sorts of mental health markers, which we currently do anyway. So I’m going to look for other types of symptoms, OCD symptoms, anxiety symptoms, psychotic symptoms, bipolar symptoms, all sorts of them to really get a full picture of brain function. But the huge change is that I am now also going to be looking at metabolic markers, biomarkers, lifestyle factors that we know impact metabolism. I’m going to be asking that person about their diet, about their exercise, about sleep, stress levels, their use of substances, their use of medications. And I’m going to be putting all of that information together in one coherent way. I’m going to try to understand what are all of the factors that are causing harm to this person’s metabolism. So that might be a bad diet and poor sleep. Maybe they’re not prioritizing sleep, they’re on their computer, they’re staying up all night binge watching Netflix, and then they don’t get enough sleep. I’m going to recognize that those are impairing metabolism. And I’m going to try to address those first before I start throwing pills at this person, and even probably before I start psychotherapy with this person. I’m going to use lifestyle factors for clear and unequivocal metabolic problems, and I’m going to see what I get.
For a lot of people, I think that’s going to solve the problem. And the beauty of this theory is that at the same time I’m addressing their depression, I’m also addressing their weight issues. I’m also reducing their risk for pre-diabetes or diabetes. I’m reducing their risk for a heart attack. I’m making this person a happier, healthier person overall. I’m treating the whole person, not just brain symptoms. I’m treating all of it. Some people may still… We may go through everything and say, “Well, we can’t really find anything wrong.” They’re following a good diet. They’re getting adequate sleep. They’re not too stressed. I’m still open to using antidepressants and talk therapy and psychotherapy, and even more invasive treatments like ECT and TMS if those are needed. But I think that the metabolic theory of mental illness opens up entirely new ways to think about what’s happening all the way down to the cellular level. And much more importantly, it opens up entirely new ways to treat these disorders and put these disorders into full remission as opposed to just reducing symptoms.
Brett McKay: Well, you were talking about talk therapy. I just had the thought, I think what might be going on there, why talk therapy is useful. We typically think, “Well, talk therapy is useful ’cause it helps you get over maladaptive thinking patterns, for example.” But I think what a lot of talk therapy does is you’re talking to someone. You have someone you can trust and talk to, which feels good, reduces stress. You learn skills, cognitive skills so that you basically reduce stress, which affects metabolism. That’s potentially what’s going on. Yeah.
Dr. Christopher Palmer: Absolutely. And I think that’s a really important point. So this theory doesn’t replace existing treatments that we know work for some people. This theory simply offers a completely new way to understand how and why something like psychotherapy or an antidepressant might be working.
Brett McKay: Yeah. And I think for someone who’s listening to this, I think this would be great. If someone has like severe mental illness, like schizophrenia, things like that, you’d have severe interventions, like maybe, “Okay, we’re going to completely switch up your diet, try keto.” Of course, you want to talk to a doctor about that. But even if you don’t have any mental health issues, I think this information explains why you should focus about eating well and exercising and reducing stress ’cause not only is it going to help your body, but it’s going to help your mind as well.
Dr. Christopher Palmer: Absolutely.
Brett McKay: Yeah. Well, Chris, this has been a great conversation. Where can people go and learn more about the book and your work?
Dr. Christopher Palmer: The one website I’ll direct people to is brainenergy.com. So brainenergy.com.
Brett McKay: Awesome. Dr. Chris Palmer, thanks for your time. It’s been a pleasure.
Dr. Christopher Palmer: Thank you, Brett, for having me.
Brett McKay: My guest today was Dr. Chris Palmer. He’s the author of the book Brain Energy. It’s available on amazon.com and bookstores everywhere. You can find more information about his work at his website, chrispalmermd.com. Also check out our show notes at aom.is/brainenergy where you can find links to resources, we delve deeper into this topic.
Well, that wraps up another edition of the AOM Podcast. Make sure to check out our website at artofmaniless.com where you can find our podcast archives as well as thousands of articles written over the years about pretty much anything you think of. And if you’d like to enjoy ad free episodes of the AOM Podcast, you can do so on Stitcher Premium. Head over to stitcherpremium.com, sign up, use code “manliness” at check out for a free month trial. Once you’re signed up, download the Stitcher app on Android iOS and you can start enjoying ad free episodes of the AOM Podcast. And if you haven’t done so already, I’d appreciate if you take one minute to give us a review on Apple Podcasts or Spotify. It helps out a lot. If you’ve done that already, thank you. Please consider sharing the show with a friend or family member who you think could get something out of it. As always, thank you for the continued support. Until next time, this is Brett McKay reminding you to not only listen to AOM Podcasts, but put what you’ve heard into action.